Interview Highlights: “The Cloud” & Living Through COVID-19 Infection with J. Thomas Vaughan Jr.5/28/2020
Interview by: Hannah Lin (CC '23)
The following is a heavily condensed version of the full interview. If you're interested, read more here. Can you describe your COVID-19 research? We have a collaboration of about 30 people—physicians, staff, faculty—across Columbia. The title of our research is COVID-19 Longitudinal Multi-ethnic Bioimaging Assessment of Cardiovascular Sequelae. Now that’s a mouthful—obviously the physicians thought that one up [laughs]. They worked hard to come up with an acronym. If you use the right letters in the right sequence, that adds up to COLUMBIA CARDS registry.
We’ll image and compare the differences between 2 cohorts: one healthy normal group and one COVID antibody positive group. We’ll use a number of different techniques to characterize myocarditis: a viral disease of the heart and resultant heart ailments.
2. To assess the effect on myocardial function of COVID-19 infection in a multi-ethnic spectrum of convalescent patients and to relate functional features to the patient important outcomes. In other words, we’re looking at a broad spectrum of people from different ethnic groups, walks of life, races. New York is great for these kinds of populations.
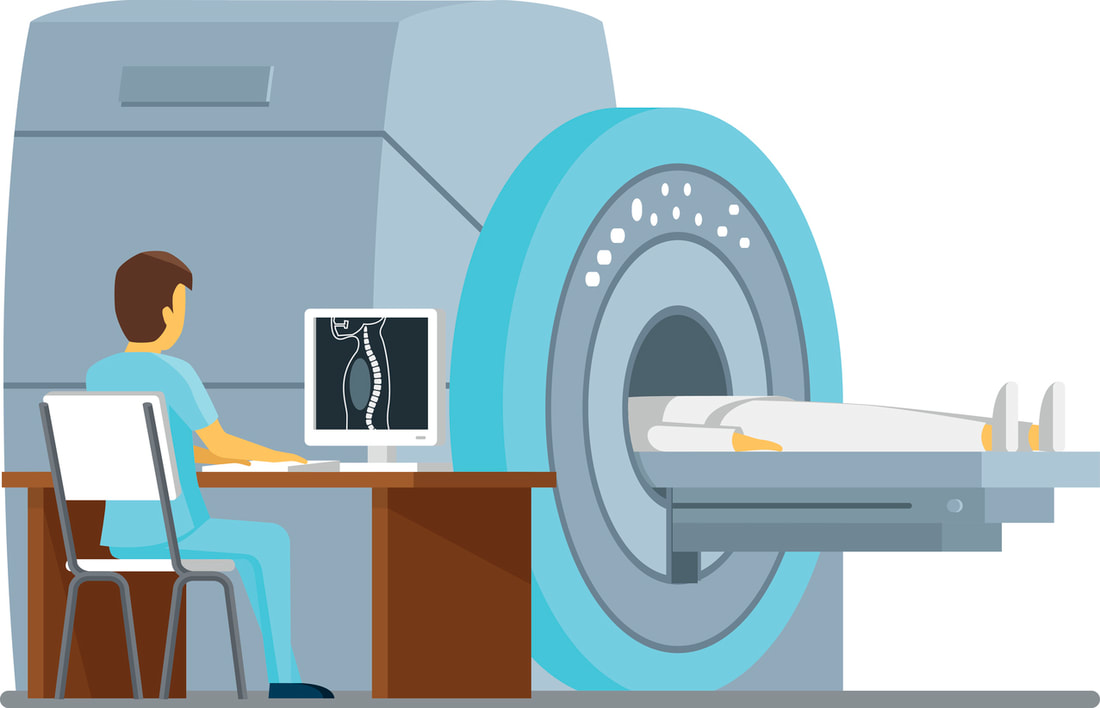
Cloud Platform. Medical imaging is 90% of the data amassed from a hospital or clinic, so it requires huge amounts of archival space.
So we really have to look to the cloud, to the future, for archiving medical image data and also for looking at that data rapidly and broadly to correlate to symptoms or anything else. Data’s the oil, the gold, the currency that so many people are beginning to trade and, frankly, makes a lot more sense than dollars and gold bars—it’s more useful. It’s knowledge. The more data we acquire from our huge, diverse patient population, the more information we have to ask big questions about certain symptoms, therapies, or differences between racial or ethnic groups, genders, or ages. Are you still keeping prior projects going?
You’ve had COVID-19 yourself. Can you talk about that experience?
So I knew I was going to get sick from something then. But at the time, frankly, it was so early—February 14th—that I thought it was a cold or flu. You know, this was back when everybody was calling this the “Democratic hoax.” Clearly, it was already alive and well in New York before February 14th; I’m proof of that.
I got home Monday night, and Tuesday morning I woke up with all the characteristic symptoms: headache, a very nonproductive dry cough, all the stomach ailments. It just felt like I’d been run over by a bus; my whole body ached. I was just thinking it was a nasty case of the flu the whole time. Everybody’s affected in different ways; to me, coughing was the worst part because I couldn’t go to sleep at night, my chest and diaphragm ached everytime I coughed, it was just painful. So I stayed doped up on ibuprofen, aspirin, everything else. There was some rumor going around for a while to “not take ibuprofen when you have COVID, because everybody that dies with COVID is full of ibuprofen” like there was some correlation. I’m like, the correlation is that if you’re dying of COVID, you need pain relief [laughs].
Unfortunately, as you see, especially in our own country, this cooperation rapidly devolved and (I’m happy to be on public record for this) because of our lousy leadership, we see an example of the human tragedy that bad leadership, a lack of coordinated government response, and a lack of international collaboration in goodwill can cause. I think we’ll be able to look back at COVID collectively and learn very important lessons across the broad spectrum of what to do and what not to do. I hope we will learn.
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |