|
By: Hannah Lin (CC '23)
You’re an infectious disease ecologist in the field of environmental health sciences. That isn’t your typical biologist or chemist. Could you explain what your title means, and also what your personal and professional path to this field looked like? As you mentioned, I’m an infectious disease ecologist, and there are only several hundred of us in the world. Those of us that identify as infectious disease ecologists are people who typically have PhDs in ecology or evolutionary biology, oftentimes also applied mathematics, and who essentially study infectious diseases from the lens of ecology and evolutionary biology. You can think of infectious diseases as predators, except they have much smaller bodies than their prey. So many of the same types of population level principles that have been used for fifty, eighty years now to investigate predator-prey relationships have now been applied to infectious diseases. Much of the same mathematics that’s used in, say, fisheries biology or predator-prey population dynamics, we apply that to infections.
That’s kind of the framing of the science. We also use evolutionary biology to study either the biology of the host, which is what my lab does in our approach to the immune system, or also the evolution of pathogens themselves. Many disease ecologists also look at the evolution of things like flu and HIV through the lens of natural selection, which is something all species experience, particularly looking at it from the disease angle. So that’s disease ecology as a field. In general, I’ve always been an ecologist. Well actually, I first started out in a genetics lab doing more evolutionary work with fruit flies. Then I moved to doing field work and endangered species work with Arctic seals, so I was working on the endangered species listing for ringed seals, which are the primary prey of polar bears (when you see pictures of a polar bear pouncing on seals, it’s those seals I used to work on). Because I was studying both mathematics and biology, I wanted to be in an area that was very mathematically leaning. In ecology, the two areas in which there is a lot of modeling applied are infectious disease work and fisheries work. I went the infectious disease route so I could use my math skills. From there, I just got really interested in working on childhood infectious diseases, did my whole PhD on polio and measles, then subsequently did work on other childhood and early life infections like chickenpox, and also worked on Zika for a bit once Zika emerged.
The last several years, my lab has also been funded to see if we have seasonal changes in our immune system that influence when we get sick and if the basis of this is a seasonal biological clock. That’s the other area of my research. I think that type of work makes a lot clearer the types of things I study as a disease ecologist. From my perspective and just in general, humans are just another mammal, so we can ask the question: how does the fact that we’re just another mammal play into our health and wellbeing? Jumping into your COVID-19 related research now, from what I saw, you and your team have been studying the immunology and transmission of this pandemic. Could you talk about your work thus far? In terms of COVID, my work has fallen into three distinct projects. One of them, which I would say is most closely aligned with the other work in my lab right now, is looking at the immune system during COVID. It’s quite clear that it’s the immune system that is doing the majority of the damage in individuals who are hospitalized, severely ill, and may succumb to the infection. For some individuals, what happens is the immune system is over-reactive and has an incredibly inflammatory immune response. Our immune system has the ability to react very strongly to an infection, but we also have processes in our immune system that keep it in check, that harness it in and don’t let it get too bonkers. But on occasion, what happens is those regulatory processes that would usually manage your immune system can fall apart for many reasons, which for COVID-19 seems to be the case. The inflammatory response just spirals out of control to such an extent that individuals can get what we call immunopathology, where you have pathology, or harm, that is being done to your body by your immune system, including things like tissue damage in the lungs, which can make people have ARDS (acute respiratory distress syndrome) and be put on a ventilator.
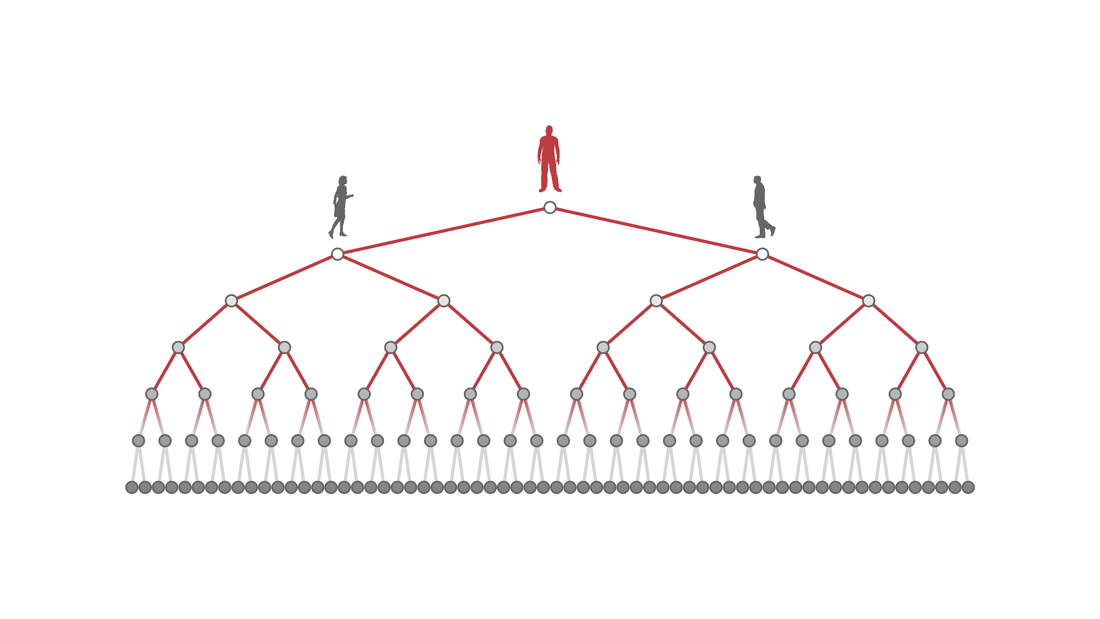
Our hope is that now by scouring the literature, by integrating data from different sources, and by digitizing data that become available (and now we’ll be using clinical data from Mt. Sinai and Columbia), we can come up with predictors for markers of our immune system that are predictive of what path the person will follow. If someone ends up in the hospital and you take a blood sample from them, we would like to be able to predict with some probability, what the chance is that this person is going to be, say, hospitalized for a week or two, recover, and be discharged versus need to be put on a mechanical ventilator and either go down the path of continued tissue damage and potentially death. As of right now, all of those paths are just dictated by your immune system. There’s not much that is able to be done on the care side of things to dictate people’s pathways that they take. Ventilators are just trying to minimize the amount of tissue damage that’s being done by helping the body supply oxygen, but they are not actually helping heal. The whole process of healing is a process of the immune system as well. The second project I have going on is transmission modeling for New York City. There are lots and lots of modeling groups worldwide that have been constructing transmission models for COVID. Where my group differs from some of those other groups is in two areas.
analyses for all these unknowns for the immune system and what’s going to happen. We need to model into the future and say, okay, if our immunity works this way, then this wouldn’t happen. If our immune system works this way, then this scenario would happen. It’s kind of like when you think about climate change scenarios: if we cut down carbon emissions this amount, then we project this will happen. Same kind of deal, but for the immune system.
Also, I’ve been working with the air pollution scientists in my department to come up with a way to measure social distancing and the slowing down of cities on lockdowns. You can easily come up with a policy; for example, the governor’s policy for lockdown in New York State where people were told to stay home. But to actually quantify and measure that is really hard unless you have something like proprietary cell phone data from every person and you can see where they’re going.
have access to. We’ve been generating algorithms that will go and take snapshots of Google Maps for every neighborhood in the city, and then puzzle-piecing those together to see how much movement there is around the city on fifteen minute intervals, going from pre-pandemic to now. We know via this type of publicly available data mining how much movement there is around the city, which can, in some ways, be a proxy for transmission potential.
My last COVID project is work that is under review right now and should be published shortly that looks at the socioeconomic and racial disparities in social distancing. When we look at the disparities based on race and ethnicity for COVID-19, there are essentially two sides of it. There’s first, thinking about what the probability is that an individual acquires the infection, and that's going to be largely dependent on how much infection is in their community, their ability to socially distance depending on what type of work they do, and also housing: if they live in a multigenerational household or if they live in a household where, if an individual is infected, they can stay away from other household members and quarantine effectively, that type of thing. So there’s that transmission side of it.
race/ethnicity, percent of essential workers, median income, and you can also get things like education, all of these things are very tightly correlated within New York City and, I would say, more broadly in the United States. If you’re poor, you’re more likely to be Black or Brown. If you’re poor, you’re also more likely to be a lower-wage worker that has to leave the home in order to work. You don’t have the luxury of staying home. All of these things come together to shape, at a community level, how much transmission there is in the community and at an individual level the risk that people face.
higher subway use during the pandemic also had higher incidence of cases, and we believe this is because of community transmission because of the social distancing inequity that's faced.
What are the broader goals of your research? Do you want to provide models for policymakers when reopening cities or something else? This is one thing that is really interesting. For instance, using the models that we’ll have for New York: inevitably, yes, policymakers are going to pay attention to that, but I’m not really in the business of modeling for policy. I’m much more in the business of modeling to understand fundamental biological processes with the aim that understanding the underlying biology will then inform translational medicine and policy. In reality, the type of work that I do, since it is more biology focused, is not meant for rapid action. If I were wanting to inform policy very directly, then I would be doing different types of modeling: for instance, modeling what the optimal criteria for shutdown and reopening would be or if you wanted to do cocooning for at-risk individuals, how you would stratify populations so some people would stay home, some would go to work, that kind of thing. Those are very directly applicable policy things, whereas my work is much more long-horizon, informing biology. As you said earlier, prior to COVID-19, you were researching other infectious diseases like polio and measles. How was the transition from researching those to this current pandemic, and did your experience with those give you unique insights into COVID-19? Yeah, definitely. The thing is that I’ve been working on the biology of acute infections for so long and coming at them from a biological angle, so it’s not all that different. COVID is just another directly transmitted infection. There is a playbook for infectious diseases. Like I was saying with predators and prey, infectious disease systems behave a certain way. There are biological bounds to how they behave.
I think I can say now that I’m the world’s expert on the seasonality of infectious diseases - that and seasonal clocks, biological rhythms in humans, are the two things that no one ever studied. Before COVID, there were so few people in the world that had any interest in seasonality of infections, and even fewer people who had ever done real empirical research in that area. When COVID hit and you had things like Donald Trump saying, “it’s going away as soon as it gets to summertime,” it was like every reporter was emailing me. I think I was uniquely placed even compared to my close colleagues because I realized I had spent so many years thinking about it that I just very innately know the nature of seasonal disease dynamics, and the math behind it is very ingrained in my brain. I noticed it with my colleagues when I thought they had the same skill set as me, but because they hadn’t specifically worked on that one area, they weren’t as well placed to think about that for this new infection. I would say my seasonality work made it so that as soon as people were asking if it was going to go away in the summer (I even had some other disease people who I would hear have that hope), I was like, no, you guys, no! I think I had just thought about that problem for a lot longer than other people had. Is there a reason why biological rhythms and seasonality haven’t really been extensively studied?
pace, getting papers out, getting grants, and such, there’s no incentive for anyone to spend their career on that unless they’re just really intellectually driven by it, which is why I worked on it.
For infectious diseases, the seasonality is very, very obvious in any infectious disease data that you look at. I would think that one of the reasons that people hadn’t studied it could just be that people don’t look at ubiquitous things, maybe? When something is so common, people don’t realize that it’s very interesting: it’s just like, the earth rotates around the sun and is tilted on its axis, so of course we have seasons! I think it’s one of those things that, since it’s so common, it gets overlooked. Lastly, what is your perspective on the future, and for a note of optimism, what gives you hope for the future? I’ll give you the good and the bad. My perspective overall is that with global climate change and the widespread destruction of natural ecosystems, including land use change and deforestation, humans, especially over the last 200-300 years, have done what is pretty close to irreversible damage to our planet. If I were just to say very bluntly, I think this pandemic has been a slap in the face from the earth to human beings. Humans have notoriously been going into natural spaces for so long where we don’t really have any business to be in. It includes forcing novel contacts with species that we usually don’t interact with. In the past, this has posed problems for us, like having zoonotic diseases that have moved into humans - things like all of our flu viruses, Ebola, HIV. But I think that in the past, there have been very few things that have just gone straight from jumping into humans right to a pandemic. Also, some of the past emergences were either more localized or they happened during a time when we didn’t have such widespread global connectedness, in terms of social media, news. Now, all of a sudden, it’s an age-old problem (age-old meaning industrial age-old): humans going places we shouldn’t be, we have a spillover from hosts into humans, and now we have this pandemic. But everyone is aware of it now, and there have been huge economic consequences and loss of life in a very short amount of time.
I think that this is going to be a turning point where either, optimistically, people realize we need to be stewards of our environment and pay attention to these things, that our actions have consequences, and therefore become those stewards that we should be, tackle climate change, tackle land use change, think about widespread extinction and pollution of our environment. And if COVID doesn’t do that, I really don't think anything else will. There’s really not much more of an acute shock that you can have from the environment onto humans than this. So I do think it does have the potential to be a turning point, but we’ll see.
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |