|
By: Makena Binker Cosen (CC ‘21)
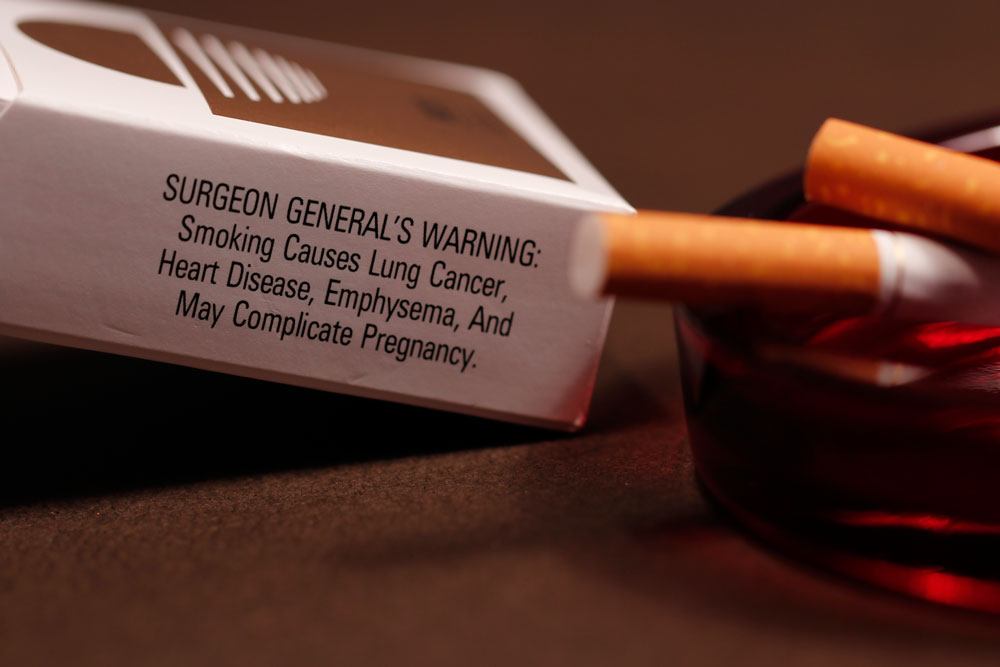
The following is a heavily condensed version of the full interview. If you're interested, read more here. What do we know about the relationship between tobacco use and a person’s risk of getting COVID-19 and developing related health outcomes?
Poor data collection may be responsible for mixed results: we don’t know how COVID patients are being asked about their smoking status or if patient responses are fully accurate. Could nicotine truly be playing a protective role because of its interactions with the inflammatory processor? That’s something basic scientists could investigate.
What inspired your COVID-related research?
Could you please describe your current research project?
What was the recruitment process for the interviews like?
We got a really diverse set of participants in terms of income level, geography, smoking behaviors, and underlying conditions. We used the screener survey results to make sure we had representation from certain groups. For example, there weren’t too many people over 70 years old completing the survey, but there were some, so we could reach out to underrepresented individuals to make sure that their voices were heard, too.
Based on your interviews, how has the pandemic influenced tobacco use behavior? Almost every person in our sample reported that their smoking or vaping behaviors changed in some way during the lockdown period. While some respondents reduced their use, increases in smoking or vaping was much more common. They shared that they felt like they needed to do this to relieve stress, boredom, and feelings of uncertainty. Participants acknowledged that smoking or vaping could put them at increased risk for COVID-19 or intensify their addiction beyond the pandemic. However, when we asked about their intentions to quit, we received a resounding “no, now is not the time.” People right now aren’t thinking about their smoking behaviors. We spoke to people who are in really, really dire circumstances — people who lost their jobs and are financially struggling; whose family members are sick or died. With the amount of stress, exhaustion, and sadness they are processing, it’s just not a priority. Many of them said, “I would love to quit. I know I should. I just can’t even think about that now. Smoking allows me to deal with all of the other stuff that is my priority right now.” As a public health professional, all of this has made me wonder what the next steps are when people have so many competing priorities other than the one we’re trying to intervene on. On a more personal level, what has this research experience been like for you? It felt nice to directly connect with people, especially during a pandemic. The people we talked to said they also enjoyed sharing their experiences about the ways COVID-19 has impacted their lives. They appreciated that people were looking into ways to better support the health and well-being of people who have various addictions. With qualitative research, you’re not just pulling data and spitting it out; you form relationships with people. Since I usually conduct quantitative studies, as a researcher, this experience has made me feel more human than any other project. Has the pandemic affected people who smoke and those who vape differently? Yes, we noticed a significant divergence in access to cigarettes and vaping products.
Sometimes, they have to wait weeks to get them delivered. If you’re addicted to something, not knowing when the next supply is going to come can be a real source of stress.
Concerningly, some vapers reported that they have gone back to smoking cigarettes because they’re just easier to get. We know that cigarettes are generally more harmful than vaping, although vaping certainly isn’t without risk. Do you have any recommendations for people using substances to cope? I now have a much better understanding of why people continue to use any of these products and I empathize with them. That said, my “public health” answer is that this is probably the best time to quit considering the risks of COVID, although I acknowledge that it’s probably the most difficult time to quit.
Where should public health professionals working towards tobacco cessation and prevention be focusing their efforts moving forward? Initiation has been slowing even before the pandemic started and my guess is that it will continue to decrease. Even so, there are people who we need to support more strongly than ever. Smoking has lost some attention among the general public because for many, it is an “invisible” problem: in a lot of people’s circles, they don’t know anyone who smokes. Although the national smoking rate is around 14%, among populations that face a lot of social and economic disadvantages, rates are just as high as they were decades ago. The smoking rate among people with mental health disorders, for example, is around 30-40%. This pandemic has exposed and magnified the major cracks in our society, particularly social injustices. A lot of people said they would need a job, financial stability, and social support to quit successfully: “once I’m at that stable place, I can do anything.” Fixing those systemic issues would hopefully lead to improvements in substance use and addiction. In some ways, disparities in tobacco use today is an outward symptom of a much larger underlying problem.
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |