|
By Kelly Butler
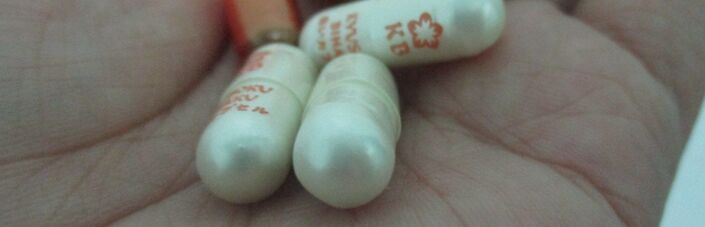
On November 13th, the Food And Drug Administration (FDA) approved Abilify MyCite, the first medication tracking system intended for public use. While the schizophrenia drug Abilify has been on the market for decades, the new Abilify MyCite system includes an ingestible sensor and wearable receiver patch, which detects when patients swallow the sensor and then transmits data to a web-based portal. Patients can always access their pill ingestion data on their smart phones, and they can also grant portal access to their doctors, family, and other caregivers. More far-reaching than a single new treatment option for psychosis, Abilify MyCite represents a new biomedical trend. For example, Peter Chai and his research team at Harvard Medical School developed digital opioids to study patient opioid use after bone fractures. Accordingly, the ethics of digital pills should be considered in the broader public health context rather than through the comparatively narrow lens of psychosis treatment. As Pam Belluck explains in a New York Times op-ed, digital pills could improve public health by increasing patient compliance. Millions of patients do not take their prescriptions as directed, causing them medical and financial harm. Failure to take medications often leads to deteriorating health and costly emergency medical treatments, including hospital admissions. Granting others access to pill-ingestion data could motivate patients to take medications as prescribed, helping them ameliorate their health and avoid financial burden. Pointing to another benefit of digital pills, Belluck also notes that the technology may be especially useful for elderly patients who want to take their medications but often forget. It could also eliminate the need for medication ingestion witnesses, which patients and nurses alike may find inconvenient and uncomfortable. Given these potential benefits, some experts have argued that digital pills have the potential to improve public health and should thus be made available to the public. Moreover, such arguments may praise the patient’s decision to use the technology and their subsequent control of who can access their data as cure-alls for any ethical concerns. While taking the digital pill and sharing data are presented as optional, there are many foreseeable cases in which these “choices” are not really up to the patient. Psychiatrist Dr. Peter Kramer nicely summarizes the technology’s potential for abuse: “While ethical for a fully competent patient who wants to lash him or herself to the mast, ‘digital drug’ sounds like a potentially coercive tool.” For example, doctors and family members may talk patients into using the tracking system, convincing them that surrendering their privacy is in their best interest. In addition, what if somebody is deemed unfit to provide consent; would that make it okay to use the ingestible sensor without his or her permission? There is thus a slippery-slope problem regarding when doctors and family members can make patients take digital medication and share their pill-ingestion data. While digital pills like Abilify MyCite have the potential to improve patient health by motivating and reminding them to take their medications, they could easily become mechanisms of coercion within medicine, a field in which patient consent is the gold standard. As the Abilify MyCite and opioid studies respectively demonstrate, medication tracking technology clearly has the potential to improve public health by increasing patient compliance and decreasing controlled substance abuse. However, digital pills come with serious ethical concerns. As scientists further develop the technology for increased public use, stringent guidelines must be established to ensure proper patient consent. For example, the guidelines could mandate that the digital pills could only be used for patients capable of consenting and that their doctor present the digital pill option in the absence of others who may impact their decision. This ethical debate about digital pill usage underscores a larger concern with biotechnology. Thanks to rapid advancements in biomedical engineering, scientists are continuously developing new medical devices that can improve patient health. We know how to use these new technologies, but the more important question is whether we should use them. Please let us know in the comments what you think of digital pills. Kelly is a sophomore in Columbia College studying biochemistry. Outside of academics, she enjoys dancing and non-profit work.
1 Comment
|
Categories
All
Archives
April 2024
|