|
By Anna Christou
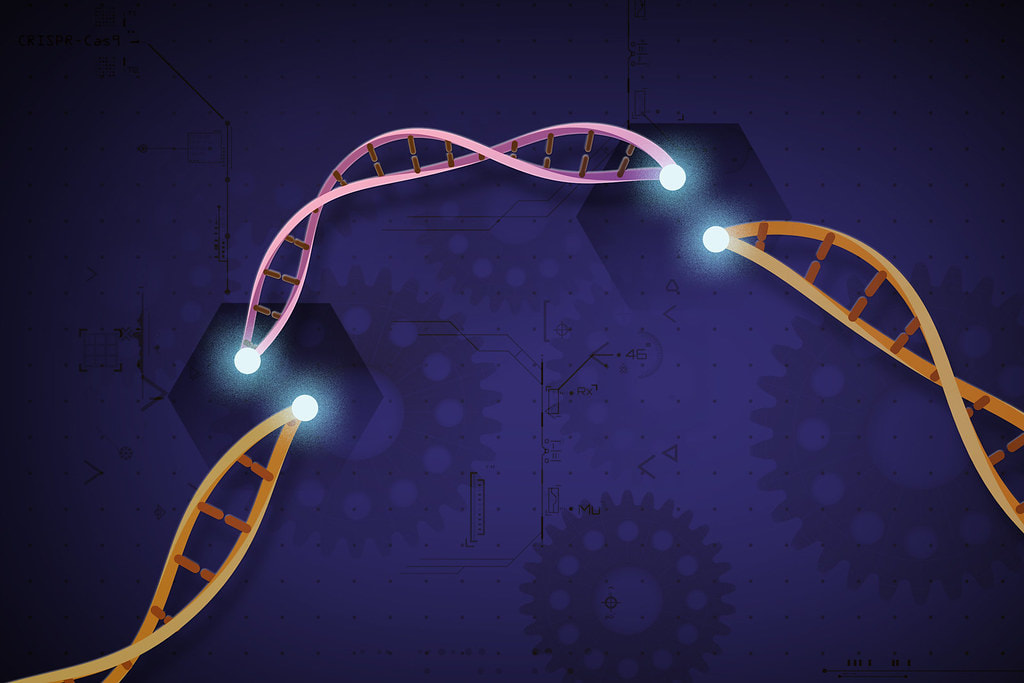
Antibiotics have impacted medicine and public health by providing a tool to control and kill bacteria. However, this powerful technology is accompanied by a wealth of problems, including resistance: when an antibiotic becomes unable to kill bacteria. Therefore, researchers have been motivated to experiment with new approaches to treating bacterial infections, including using gene-editing therapy. Resistance has made treating bacterial infections using antibiotics a widespread challenge. According to the Centers for Disease Control and Prevention, at least 2 million people are infected with antibiotic-resistant bacteria in the United States each year, and at least 23,000 people die from these infections. This is particularly an issue in hospitals, as according to the National Institutes of Allergy and Infectious Diseases, about 90,000 of hospital patients who develop an infection die each year as a result. This large problem all comes down to a classic case of natural selection and survival of the fittest. Specifically, in a population of bacteria, there is natural variation in traits, including genes that relate to survival. Because of this variety, some bacteria have the ability to withstand being killed by antibiotics. As a result, these lucky bacteria with the genes to withstand antibiotic treatment will persist and survive longer. Therefore, in the population, the bacteria with the resistance gene will have more opportunities to reproduce, further propagating the presence of the resistance gene. Misusing antibiotics, such as by not finishing a full course of shots or pills, can exacerbate this problem; rather than kill the entire population of bacteria, the antibiotic only kills some of them and leaves the resistant ones to multiply. Over-prescribing antibiotics for viral infections which are not treatable with antibiotics also fosters resistance. If a population of bacteria are targeted by a large amount of antibiotics, the resistant bacteria will be more likely to stand out and survive, propagating the resistance gene. Because overusing antibiotics further contributes to resistance, researchers have recently been working to attack bacteria using novel mechanisms. For example, there has been some research on the use of viruses, which selectively target bacteria, but not human cells—a technique called bacteriophage therapy. Furthermore, researchers at the New York University School of Medicine have recently discovered that they can use the gene-editing technique CRISPR/Cas9 to kill bacteria, specifically Staphylococcus aureus bacteria. The gene-editing technique CRISPR/Cas9 targets pathogenicity islands, which are sections of bacterial DNA that make the bacteria more harmful. Specifically, pathogenicity islands contain toxic proteins that when recognized by the immune system, release inflammatory molecules. A large production of these inflammatory molecules cause symptoms of infection, including organ failure and shock. Therefore, these researchers used CRISPR/Cas9 to modify these pathogenicity islands by either removing or blocking them. CRISPR/Cas9 is a system, naturally present in the bacterial immune system, that has been developed as a technique to target genes and to consequently delete or replace them. The system consists of two components: a Cas9 enzyme that acts as “molecular scissors” to cut the targeted gene, and a guide genetic sequence that directs the Cas9 enzyme to the gene to be cut. The scientists injected CRISPR/Cas9 into mice and tested two different, but related, versions of this system. In the first version, after being directed to the target pathogenicity island by the guide sequence, the Cas9 cuts the pathogenicity island, which kills the bacteria. In the other version, the Cas9 enzyme reaches the DNA but, rather than cutting it, just latches onto the gene. Holding onto the island blocks it, making the bacteria less effective at causing infection. The researchers then tested these results by injecting the gene-editing system into mice. Both versions of the CRISPR/Cas9 system—cutting and blocking the islands—were effective in controlling the development of infection in mice. Specifically, animals that received either of these versions of the treatment were prevented from developing an abscess, which is swelling that results from a bacterial infection. Also, S. aureus bacteria were injected into the body cavities of mice that received the first version of the gene-editing system, which killed the bacteria, in order to study how well mice could withstand infection. The mice that received the therapy that cut bacterial DNA and killed the bacteria survived the injection of these bacteria. However, the researchers found that some of the bacteria could still be resistant to this therapy, suggesting that resistance may still be a challenge that needs to be overcome. Through the ability to target different pathogenicity islands, gene-editing offers more possible solutions that likely will target the bacteria in more effectively, rather than just using one antibiotic. Therefore, CRISPR/Cas9 provides another way of treating bacterial infections without the use of antibiotics. By attacking bacteria from within through pathogenicity islands, gene-editing offers the potential for more varied targets, which might reduce the likelihood of resistance.
0 Comments
By Kyle Warner
Nuclear power generation stems from the process of splitting uranium-235 atoms, otherwise known as nuclear fission. When an atom undergoes fission, a significant amount of energy is released in the form of heat, which can then be used to produce steam that spins a turbine and produces electrical energy. Despite the relative simplicity and efficiency of this process, the word “nuclear” still comes with many negative connotations: power plant meltdowns, long-term nuclear waste, disease from radiation exposure, and potential warfare applications. Although these consequences should all present significant cause for concern, a closer look into the science behind nuclear suggests a safe, sustainable future for the power source. Chernobyl (1986) and Fukushima (2011) are the two most significant power plant meltdowns in recent memory. Despite media portrayal of significant radiation from these events, the total amount of ionizing radiation from the Chernobyl and Fukushima accidents, combined with the radiation from atomic bomb testing in the 60s and 70s, totals just 0.3% of global surface radiation. This is because most of the radiation we experience comes directly from the Earth, atmosphere, and buildings that surround us. For example, Colorado experiences more net annual radiation than the surrounding areas of Chernobyl and Fukushima as a result of low atmospheric shielding and high concentrations of natural uranium in the ground. Additionally, the meltdowns at Chernobyl and Fukushima have shown no direct evidence of impacts on fertility, birth defects, or infant mortality. There is no correlation between the radiation and any form of cancer except for thyroid cancer, commonly perceived as one of the most treatable forms. Of the fifteen deaths caused by thyroid cancer from the Chernobyl accident, the majority were from residents of rural areas without access to proper treatment. In addition to the limited risk associated with the radiation, a comparison of nuclear power with other common energy sources further suggests that nuclear has the advantage. Contrasting the energy produced by equivalent mass of different materials paints a clear picture: one kilogram of coal can produce 8 kWh of electricity, one kilogram of oil can produce 12 kWh, and one kilogram of uranium-235 can produce 24,000,000 kWh! For reference, a single consumer in the United States requires approximately 10,766 kWh of electricity per year. A quick back-of-the-envelope calculation shows that one kilogram of uranium-235 can provide energy for almost 2,250 United States residents a year while an equivalent mass of coal or oil would fail to simply meet the needs of a single resident. Nuclear power also generates zero greenhouse gas emissions, whereas the burning of fossil fuels releases significant amounts of air pollutants and greenhouse gases such as carbon dioxide and methane which are the primary culprits behind climate change. While renewable sources such as solar and wind are effective at limiting greenhouse gas emissions, the efficiency of energy production pales in comparison to nuclear as they require significantly more land for a similar output and are intermittent supplies (the Sun is not always shining and the wind is not always blowing). Although battery storage would allow for solar and wind to produce constant energy and is a rapidly growing field that should continue to be developed, there remain significant hurdles to achieving complete reliance on renewables. There are many countries in support of the development of sustainable nuclear power for the future. The Generation IV International Forum (GIF) is a coalition of fourteen countries, including the United States, who share the common goal of carrying out the research needed to establish performance capabilities for the next generation of nuclear power systems. Of the hundreds of nuclear reactor designs presented to the GIF, six were selected as the basis for future development based on the following sustainability standards: reducing the amount of time waste remains radioactive from millennia to centuries, improving energy yield by operating at higher temperatures, increasing the variety of fuels used in operation, allowing for the reuse of nuclear waste as fuel, and eliminating applications for weapons technologies. These six reactor designs fall into two general categories, thermal reactors and fast reactors, and as a group are effectively known as Generation IV reactors. The human error that contributed to the incidents at Chernobyl and Fukushima would be effectively eliminated in these Generation IV reactors through an automatic shutdown system to be initiated in cases of emergency. The GIF intends to have these reactors deployed commercially between 2030-2050 depending on their varying degree of technical maturity. Despite the promise these reactors show as an end-all solution to the energy crisis, it remains a necessity to continue the growth of renewable energy sources to displace fossil fuels and limit climate change-inducing greenhouse gas emissions while Generation IV reactors are being developed. If renewables maintain their positive trajectory and the commercialization of Generation IV reactors is a success, the future of energy will have eliminated greenhouse gas emissions and see significant improvements in both efficiency and safety standards. 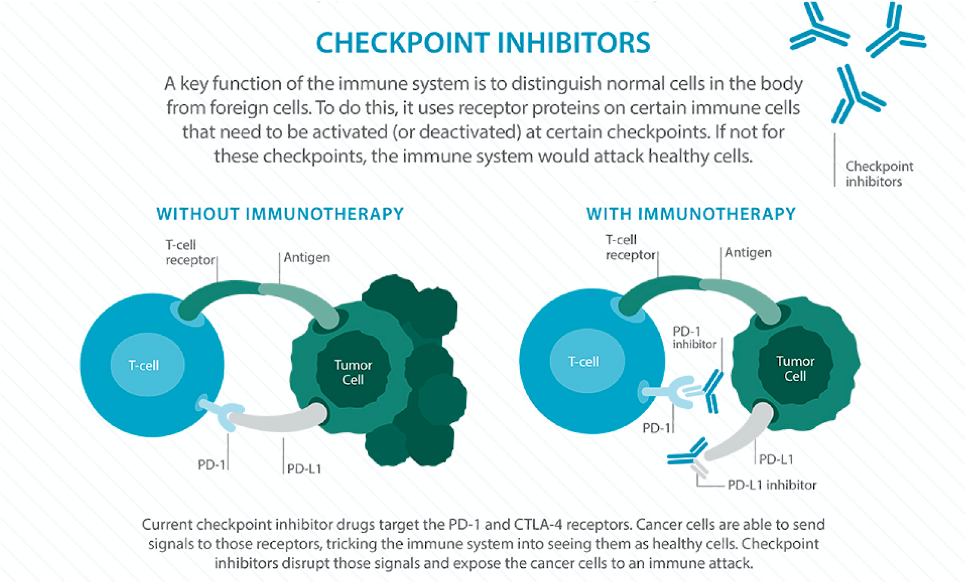 By Clare Nimura Why can’t your immune system fight cancer the same way it fights a common cold? The immune system is supposed to recognize the bad things in your body, eradicate them, and let you go on with your life, healthy. Why does the body’s defense system fail when it comes to cancer? This month, the Nobel Prize in Physiology or Medicine was awarded to James P. Allison and Tasuku Honjo for their work on immunotherapy. These two doctors independently discovered the importance of checkpoints (specifically CTLA-4 and PD-1) in manipulating the immune system and revolutionized the field of cancer treatment. Before we can appreciate how monumental these discoveries are, we need to take a step back: how does the immune system work? What even is a checkpoint? The immune system is composed of cells, tissues, and organs that coordinate to attack antigens, or any foreign or dangerous substance in the body. Some immune cells have the job of identifying antigens and calling for a larger immune response. These cells tag the antigen with small proteins called antibodies, which act as a “destroy me” tag recognizable by other immune cells. Each type of antibody latches onto a specific antigen. Despite this elaborate defense system, cancer has found a way to slip past the immune system’s careful watch. How does it do it? Essentially, cancer cells have the ability to flip the “on/off switch” of immune cells, hiding themselves from being recognized as harmful. These “on/off switches” are proteins on the immune cell surface called checkpoints. Many cancer cells produce complementary proteins on their surfaces that bind to these checkpoints, which send the signal to the immune cell saying, “I’m harmless!” and prevent any immune response. This is a problem: if the immune system cannot recognize the cancerous cell, it cannot do anything to destroy it. What if there was a way to train your body’s immune system to recognize cancerous cells and give it the strength to overcome the disease? Well, there is a way: immunotherapy. Immunotherapy is an exhilarating frontier of cancer treatment, voted “Breakthrough of the Year” by Science Magazine in 2013. It harnesses the body’s own immune system, super-charging it to battle cancer. There are three main categories of cancer immunotherapy: adoptive cell transfer, monoclonal antibodies and checkpoint inhibition. Drs. Allison and Honjo won the Nobel Prize for their work specifically on checkpoint inhibition. Let’s take a closer look at how checkpoint inhibition works. When cancer cells “turn off” immune cells, they apply the brakes to the immune system. Checkpoint inhibition releases these brakes, allowing the immune cells to recognize the cancer cells as harmful and to function at full capacity. A new class of drugs called “checkpoint inhibitors” acts by binding to—and effectively disabling—the checkpoints on the immune cells or the proteins on the surfaces of the cancer cells. If these proteins cannot interact with each other, then the immune cells cannot be “turned off.” There is now a whole range of drugs that block different checkpoints, allowing the immune system to function without receiving inhibitory signals from cancer cells. Basically, checkpoint inhibitors destroy the cancer cells’ hiding technique so the immune system can do its job. Immunotherapy is an exciting frontier of medicine that is emerging into mainstream treatment. So far, it is FDA approved for melanoma, lung cancer, head and neck cancer, Hodgkin lymphoma, kidney cancer, bladder cancer and Merkel cell carcinoma. So far it has been most effective in melanoma and non-small cell lung cancer, with some clinical trials showing almost doubled overall survival. Other clinical trials are even exploring the prospect of using immunotherapy in other diseases like Alzheimer’s and multiple sclerosis. However, like any other treatment, immunotherapy is not a miracle solution and does not come without drawbacks. Patients often experience flu-like symptoms or inflammation as side effects—consequences of an overactive immune system—and the treatment is not universally effective. Different types of immunotherapy also work better for different cases. For example, adoptive cell transfer and monoclonal antibodies involve more complex procedures but provide more specificity in treatment, whereas checkpoint inhibitors use a simpler mechanism and boost the immune system generally. Endless questions still surround immunotherapy: Does it work best alone or in combination with other cancer therapies like chemotherapy, radiation, and surgery? Why doesn’t immunotherapy work for every patient? What are the long term effects of immunotherapy? Due to these and other uncertainties, immunotherapy is typically a “second-line” treatment, introduced after patients have progressed on the traditional treatments of chemotherapy, radiation, and surgery. While there is still much to discover in the field of immunotherapy, the recognition of Dr. Allison’s and Dr. Honjo’s work marks the beginning of a new era of cancer treatment, one where our very own immune system becomes a valuable weapon. Maybe someday we will be able to treat cancer the same way we treat a common cold. By John Wang
You know you should’ve gone to the gym instead of lying on your couch and watching that last episode of Game of Thrones. But sometimes the warmth and comfort of a blanket burrito is too precious to give up for anything else in the world. According to researchers at the University of British Columbia, you might be avoiding gym day not only because you are good at coming up with excuses, but also because of your predefined biological features -- in particular, the massive, complex organ sitting on top of your shoulders -- your brain. Matthieu Boisgontier, the leading postdoctoral researcher at UBC’s Brain Behaviour Laboratory, called this the “exercise paradox”; that is, knowing that physical activity is significantly more beneficial than inactivity, we still incline towards the latter. Boisgontier and his colleagues hypothesized that there could be a hardwired mechanism embedded in our neural circuitry that favors laziness over exercise. The researchers recruited 29 young adults who were tasked to control an on-screen avatar in front of a computer. They flashed single images depicting either physical activity or physical inactivity, and asked the subjects to move the avatar as quickly as possible toward the pictures of physical activity and away from the pictures of physical inactivity. Then, subjects repeated the experiment, but with opposite goals -- that is, moving the avatar towards the lazy pictures and away from the active pictures. Meanwhile, noninvasive electrodes recorded their brain activities using electroencephalography, which picks up the tiny electrical currents generated by the active neurons. Boisgontier found that participants were generally faster at moving toward active pictures than moving away from lazy pictures, but the electroencephalograms showed that doing the latter required their brains to work harder. This increase in activity is nonetheless an unconscious one, where the brain regions that are responsible for automatic processes were responding the greatest when challenged with physical activities. In other words, the brain has to work extra hard to counteract the innate response that discourages physical activities. One explanation suggests that there may be an evolutionary benefit to being lazy. According to Boisgontier, “conserving energy has been essential for humans’ survival, as it allowed us to be more efficient in searching for food and shelter, competing for sexual partners, and avoiding predators.” Therefore, natural selection preferred humans who were innately good at conserving energy when they didn’t need to expend it. What Boisgontier’s work shows is that overcoming this biological urge to be lazy is expensive. “The exciting novelty of our study is that it shows this faster avoidance of physical inactivity comes at a cost—and that is an increased involvement of brain resources,” says Boisgontier. “These results suggest that our brain is innately attracted to sedentary behaviours.” This view supports a study by University College London published last year, which found that our brains may trick us into unconsciously viewing a low-effort option as preferable over options that require more effort. Perhaps this provides the perfect excuse for not going to the gym. After all, it’s not that your will doesn’t want to; it’s your uncontrollable, subconscious self. If we want to avoid a philosophical discussion on whether free will exists or not, perhaps we can turn to science for insights on plausible solutions. Numerous studies have demonstrated the brain’s ability to rewire. In fact, the brain is able to reorganize and restructure itself by creating new and strengthening old connections between different neurons and brain regions when needed. There are cases where patients are able to regain the function of their damaged brain regions through the adaptation of remaining healthy regions. Specifically, cell death due to injury immediately leads to heavy modifications in the neural network as neurons engage in synaptogenesis, which is the creation of new nervous connections. This entire process, also known as neuroplasticity, has allowed numerous stroke survivors to slowly regain their lost functions, such as speech or motor functions. Similarly, there are also neuro-cognitive training programs developed for recovering addicts, aiming to facilitate the reconstruction of a healthy and independent reward circuit from their drug abuses. Therefore, we are not doomed to our couches for the rest of our lives just because our brain isn’t “optimized” to encourage physical activities. As much as the brain is able to encourage laziness, it is equipped with even more tools to encourage actions. If we consciously associate exercising as a positive, rewarding activity, we may then drive other neural circuits to override the “lazy” one. Furthermore, we can involve outside factors such as friends or training coaches to help us develop healthy habits. After all, whether it’s gobbling potato chips in front of the TV or sweating on a treadmill, it is up to you to decide which one to choose. John Wang is a sophomore in Columbia College studying Computer Science and Neuroscience & Behavior. He is currently a research assistant in Yuste Lab, Neurotechnology Center, as well as a member of the Columbia Neuroscience Society. By Mariel Sander
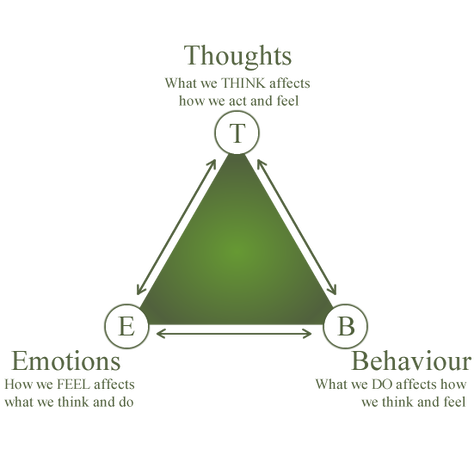
When considering treatments for mood disorders like depression or anxiety, people usually think of medications like Prozac or Zoloft - medications that necessitate a lifelong dependence on fluorescent orange bottles and daily pills. On the other hand, while psychotherapeutic treatments exist, individuals often imagine them as ineffective, unscientific, and outdated. Last fall, my friend made the decision to take a year off from school to focus on improving his mental health. He enrolled in a program focused primarily on teaching participants how to implement a kind of psychotherapy called cognitive-behavioral therapy (CBT). CBT is a relatively new, promising psychotherapy that’s been shown to promote positive neural changes and long-term mood improvements with the same efficacy as pharmacotherapy. As the name suggests, CBT is a combination of cognitive and behavioral therapeutic methods. There is a marked focus in understanding one’s own cognitive processes and how these habits affect behaviors. This approach is often visualized in a triangle schematic in which emotions, thoughts, and behavior are interconnected. What differentiates CBT from other psychotherapies is its emphasis on patient-led, practical problem-solving. A traditional psychotherapeutic approach helps the patient search for underlying causes of their illness by examining possible childhood traumas and influences. However, in CBT, the therapist simply teaches the patient to address their difficulties in an immediate and self-sufficient manner. One common technique taught in CBT involves becoming more aware of negative patterns of thought called “cognitive distortions.” One cognitive distortion would be “mind-reading.” Let’s consider an example of this distortion. Your close friend cancels on your plans to see a movie together. If your most immediate thought is “they must have canceled because they don’t like me and think I’m weird,” you’re falling into the pattern of “mind-reading.” You think you know what someone else is thinking about you, even when in reality there could be many other reasons they chose to cancel. In CBT, a therapist would teach the patient about these cognitive distortions and how to become more aware of them. CBT focuses not on delving into the patient’s past, but on finding future solutions. The patient must be self-motivated and willing to change aspects of their thoughts and behaviors to cultivate a better, healthier mindset. Over the years, CBT has been effective in treating more than just depression. It has also been proven to have the same efficacy as and lower rates of relapse than pharmacotherapy for anxiety, post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), and phobias. A 2005 study found that PTSD patients typically have trouble with social cognition, particularly in the areas of empathy and forgiveness. After CBT, the patients showed increased activation in the left medial temporal gyrus and posterior cingulate gyrus, two parts of the brain linked to empathy and forgiveness, without the use of traditional medications. Additionally, CBT was shown to be effective for treating OCD in a study where a group of afflicted individuals underwent CBT, while another group underwent the traditional pharmaceutical treatment with fluoxetine. Neuroimaging showed that both CBT and pharmaceutical groups displayed a decrease in activity in the right caudate nucleus, which consequently reduced the expression of OCD symptoms. There was, however, a small difference noted: the group treated with fluoxetine demonstrated a decrease in thalamus activation, while the CBT group did not. However, there haven’t been definitive studies linking decreases in thalamic activation to the improvement of symptoms. While CBT does have real, quantifiable benefits, there are some critical faults, as reported by my friend. “It was exhausting and daunting to think that from now on I had to change my thoughts and second guess myself,” he said, after weeks of working with therapists and learning CBT techniques. “It definitely isn’t easy.” As my friend's experience suggests, CBT requires that patients invest an incredible amount of work, persistence, and self-motivation to ameliorate their disorders. Nevertheless, research suggests CBT can be effectively implemented even in cases of severe depression. In these cases, CBT is often also combined with medication to achieve more rapid results. Despite CBT’s proven efficacy, most state mental health systems have neither instituted nor funded it. This could be due to the misconception that medication is the only route to promoting positive neural changes or that merely forming different habits, as in CBT, doesn’t substantially affect the brain. CBT provides a promising route to a more patient-focused form of treatment, providing insight into the patient’s own thought patterns and allowing them to better understand, and thus improve their overall mental health. “With lots of practice, the skills I learned throughout therapy have changed my overall mood in drastic ways,” said my friend, upon completing his combined CBT and pharmacotherapy program. “Surprisingly, CBT has been life-changing for me.” By Sophia Ahmed
The New York Subway system is one of the most extensive subway systems in the world. With nearly 1.8 billion riders every year, the subway system is an integral part of what makes New York City tick. However, ever since the 1970’s, because of perpetually deferred maintenance, riders have faced a growing number of delays and derailments during their journeys beneath the city. As pressure to fix these issues rises, the Metropolitan Transportation Authority (MTA) seemingly causes more problems than it fixes when it closes lines for repairs. The inconveniences of the repairs are often blamed on the increased ridership of the subway system and its unique 24/7 service. However, these issues, primarily signaling issues, stem from the subway’s technological faults. By investing in smarter repair strategies, better signaling systems, newer train carts, and an updated payment system, the MTA can return the New York Subway system to its glory. Furthermore,the MTA does not need to come up with novel ways to best act on investments; it can build on ideas from subways systems around the world. The aged signaling system in New York’s subways epitomizes the MTA’s failure to modernize the system. The signaling system is the backbone of the subway system: it tells operators the location of every one of the 6,418 subway trains so they know when and where to move. Much of the system, however, was built before World War 2 and relies on outdated electromechanical switches that flip every time a train passes over them. Because these switches are largely mechanical, there is a delay in the time that it takes a signal to reach an operator, making location information inaccurate and causing trains to have a larger, unnecessary gap between each other. Additionally, because the switch-signal infrastructure is so old, the switches are deteriorating, and when they break, the trains will stop, regardless of other train positions. The signal system’s combination of delayed information and the deterioration of infrastructure causes 13% of all subway delays. Moreover, the aged signaling system gives riders inaccurate information about when to expect their train, increasing the inconvenience of the already difficult subway system. The MTA can learn from London Tube operators on modernizing its signaling system. With London’s new signals, more trains can operate per line (on some lines, the number of trains has increased by 10) and each station has a train pulling in every one to two minutes. Altogether, these changes decrease the burden of increased ridership and leads to a more efficient system. But the overhaul of the signaling system was not an easy feat for London officials: closures and 7 billion dollars were poured into the renovations. When speaking to the New York Times, Mark Wild, the managing director of the Tube, said that updating the first lines was a learning process, yet as officials and workers learned more about the updates, modernization became easier. After just three years, the Tube had completely revamped its signal system, compared to the MTA’s estimation of New York’s signal system update being completed in 2045. The London signaling system is now computerized with electronic transponders instead of switches, meaning that train-location information is no longer delayed. The system is also centralized, allowing for easier identification of issues, especially if a problem involves more than one train line. By seeing how signaling has improved the Tube, as well as the difficulties that London officials encountered, the MTA can devise a strategy that would maximize installation productivity. No matter the strategy, one thing is clear: improving signaling systems is crucial for increasing the efficiency of New York’s subway. Modernizing the signal system also would require upgrading train cars, which are also a key contributor to the subway’s inefficiencies. Train cars can be improved primarily in two ways: automation and space maximization. Current New York subway trains are each operated by a two-person team. By cutting down this number to one or even zero, the MTA can save millions of dollars in wages per year. Automation will also allow trains to have shorter stopping times at stations, thus decreasing ride and wait times. Automating subway cars is not limited to the driver either. In Beijing’s subway system, the train doors open automatically in case of a fire, which can speed up evacuation times. Additionally, these cars also have sensors on their doors that alert station attendants when too many people are trying to board the train as the doors are closing. Preventing people from wasting time trying to pack onto crowded trains further reduces travel time. Besides modernizing the rails through both the signaling systems and the cars, the MTA has yet another option to increase travel efficiency: improving the fare-collection stations. Current stations often require riders to swipe in multiple times and entry is limited to those with a MetroCard. On the other hand, stations in London and Beijing allow riders to tap their debit cards, credit cards, Metrocards, and even smartphones to pay the riding fare. This will shorten both lines to get Metrocards and to the platform, allowing for a more efficient commuting experience. Additionally, if MTA could integrate live data-collecting systems into updated turnstiles, riders would get updated data on how crowded stations are and make better-informed travel decisions. Live data could also allow the MTA to integrate demand-based fares into its system where fares at busy times would rise slightly, thus giving many riders an incentive to ride at a slightly less busy time. This could also help MTA collect additional revenue. Clearly, the core issues of overcrowding and delays in the New York Subway system can be solved with the appropriate application of technology. Cities around the world have been improving their subway systems and the MTA can use these cities as a blueprints for its plans. Although high costs remain an obstacle in implementing these improvements, passing the plans through political hoops can be much easier with the presentation of success stories from other countries. Most importantly, technological upgrades improve the subway riding experience to make New York a more connected, prosperous city. By Alice Sardarian
One may be familiar with the red flowers of the delicate poppy plant adorning coats and wreaths on Armistice day, otherwise known as Remembrance day. Most, however, are not familiar with another poppy that has made extensive contributions to the pharmaceutical industry and, unfortunately, has also become a major global health threat. The Papaver somniferum, or opium poppy, is the natural source of opiates. The plant, originally native to the Eastern Mediterranean, is now cultivated all over the world. Afghanistan is the largest producer of opium poppy and opiates: in 2017, the nation produced 9,000 metric tons of opium, which accounted for about two thirds of the global area of illicit opium poppy cultivation in 2016—an area about the size of 427,000 football fields combined. Most of the opiates flooding United States markets, however, originate from South American countries, like Colombia and Mexico. Opioids are composed of three main psychoactive ingredients: morphine, codeine, and thebaine. Common opiates are derived from these main ingredients. For example, heroin is an ester that is formed from morphine. Other opioids are synthetically engineered and significantly more potent, such as fentanyl. Opioids work by binding to opioid receptors in the brain, activating G protein-coupled receptors, and ultimately resulting in a cascade of dopamine. The reception of the dopamine neurotransmitter allows the user to experience pain relief, euphoria, lethargy, and sedation. These are the intended effects of the drugs’ short term use. However, repeated, long-term use of opioids diminishes the sensitivity of opioid receptors. Users, then, require higher doses of the drugs in order to achieve the pain relief and pleasure acquired from their original doses. The physiological dependence and addiction that arise from this continuous need to activate the brain’s reward system has prompted a global health crisis like no other. Opioids are highly addictive, easily accessible, and frequently prescribed. Under these conditions, opioids have become the most abused drugs in the world. The 2015 the World Drug Report indicated an 11% increase in opioid seizures worldwide. Deaths due to opioid overdoses in the United States tally more than 115 individuals per day and continue to increase every year. These deaths pose, for the US alone, an economic burden of over $78.5 billion a year. In order to combat and to address the opioid overdose crisis, authorities have rallied for the inclusion of civilians in the global healing process. For example, Dr. Jerome Adams, the US surgeon general, recently recommended that more Americans, in all walks of life, carry naloxone, a life saving drug easily administered to reverse frequently fatal opioid overdoses. Naloxone administration was previously limited to hospital settings, and a trained medical provider was required to deliver the drug in its syringe form. Today, naloxone is available in a quick and easily inhalable format, under the brand name Narcan. The drug blocks the opioid receptors and, in just two minutes, restores the victim’s failing respiratory capacity. Narcan administration may cause the victim to experience extensive nausea and vomiting, but these are side effects that pale in comparison to the drug’s life saving benefits. Narcan is now available at major pharmacies and is covered by most insurance programs. Anyone can easily visit a naloxone distributor in the vicinity and acquire the life-saving drug. New York City has implemented numerous programs in an attempt to combat its opioid epidemic. About three New Yorkers die every day as a result of an opioid overdose, a number that is three times the city’s murder rate. In March 2017, Mayor Bill de Blasio started the HealingNYC initiative in an effort to accelerate a city-wide response. A primary component of the program is the “Save a Life, Carry Naloxone” campaign. Signs depicting ordinary, citizen heroes are scattered all over the city, above subway entrances and across billboards. They highlight the powerful, life-saving actions of neighbors, family members, and even strangers. New Yorkers are saving New Yorkers. With simple instructions, a non-medically trained, ordinary New Yorker, can reach out to a potential overdose victim and administer the life saving naloxone. Simply put, more individuals can help save the lives of those who may lack access to medical professionals, are disenfranchised, or are simply afraid of authorities. Although the quick and effective treatment of overdoses is essential to saving lives, it is equally important to prevent the overdoses from occurring. Fentanyl is a synthetic opioid that is about 100 times stronger than morphine, and is responsible for 70% of overdose deaths. It is often found in illicit drugs, added by dealers unbeknownst to users. Fortunately, a $1 test strip developed by a Canadian company can help detect the presence of Fentanyl in tainted drug supplies. By targeting illicit drug sources and removing more dangerous products from the drug market, opioid overdoses could be drastically reduced. In addition to preventing excessive Fentanyl exposure, it is paramount to replace or at least minimize opiate prescriptions, which would reduce the risk of developing an opioid dependence. This has been quite difficult, as opioid manufacturers have heavily promoted their products and provided monetary incentives to physicians who prescribe these pain killers. From 2014 to 2016, the pharmaceutical industry, as a whole, spent more than $102 million lobbying members of Congress to prevent the Drug Enforcement Administration from regulating the industry. When physicians and lawmakers receive incentives to keep opioids readily available and to prevent better pain management practices, it is difficult to curtail the prescription of opiates, and the consequent drug dependency and patient addiction that stems from it. Some positive change is taking place to counter the profit-based trend of over prescribed opiates. Dr. Alexis LaPietra of St. Joseph Hospital, NJ, has devised the ALTO program to begin the replacement of frequent opiate prescriptions. The ALTO program outlines alternatives to opiates in the treatment of various medical conditions. To address musculoskeletal pain, for example, instead of opiates, Dr. LaPietra recommends acetaminophen, ibuprofen, muscle relaxants, and trigger point injections. These treatments are effective at relieving pain, while circumventing the excessive distribution of and use of opiates. Since the implementation of the ALTO program in 2016, the Emergency Department at St. Joseph’s has reported a 50% decrease in opiate use and prescriptions, a change that illuminates the efficacy and potential success of alternative pain management approaches. While physicians like Dr. LaPietra are beginning to change the trajectory of this epidemic by not only questioning their practices, but also by drastically changing their treatment strategies, conscientious, educated citizens are also raising awareness and taking further actions against this crisis. Carrying naloxone, emergency medical responders, police officers, librarians, and community members, acting under the Good Samaritan Law, have come together to help save more lives. Today, tragic fatalities from opioid overdoses touch many American lives. This public health emergency is of an epic magnitude, and impacts people from all walks of life. Hence, there is an urgent need to address it on many levels, using multiple strategies and approaches. In order to combat and to eradicate the epidemic, local and nationwide entities must come together to create change on all fronts. These strategies must include and not be limited to: prevention education, decreasing the prescription of opiates, strengthening legislation, weakening big pharmaceutical lobbying, and, most importantly, providing drug users with the support, intervention, and tools necessary to keep them safe and alive. Alice Sardarian is a sophomore at Barnard College majoring in Physiological & Organismal Biology. She is managing editor for the Columbia Science Review. |
Categories
All
Archives
April 2024
|