|
By Liza Casella
Psychedelic mushrooms, colloquially known as magic mushrooms or shrooms, have a long and complicated history. While people used them in religious and cultural rituals for centuries, these mushrooms only caught the attention of the scientific community during the mid-twentieth century. Accordingly, scientific efforts began to investigate the effects of various psychedelics on the human mind. Psychedelic mushrooms also appealed to the general population, leading the era’s overzealous administration to classify them in 1971 as a Schedule I Drug — one that has “high potential for abuse and the potential to create severe psychological and/or physical dependence…[with] no accepted medical use.” This classification, however, may be erroneous. Psilocybe cubensis is the most common member of the family of psilocybin-producing mushrooms. Psilocybin is the compound responsible for the “trip” that follows the ingestion of psychedelic mushrooms, which belong to the drug class of hallucinogens. Inside the body, psilocybin is chemically converted to psilocin, an active agent within the central nervous system. Psilocybin is structurally similar to serotonin and, once converted to psilocin, it serves as a partial agonist for serotonin receptors by acting like serotonin and affecting the serotonergic transmission system, which regulates one’s mood. Moreover, while psilocybin does not interact with dopamine receptors directly, it leads to downstream effects that increase the amount of dopamine in the basal ganglia, the area of the brain responsible for motor control, behavior, and emotion. Ultimately though, the exact pathways through which psilocybin affects the brain are still being elucidated. Furthermore, the effects of psychedelic mushrooms vary depending not only on the species and amount, but also the person ingesting them and the setting in which they are ingested. After consumption, people may experience euphoria, epiphany, visual effects, distorted perception of time, giddiness, dissociation, disorientation, and elevated energy. On the other hand, they may also experience anxiety, panic, and sadness, which are considered characteristics of a “bad trip.” In the past decade, there has been a resurgence in research involving psychedelics, primarily for their potential in treating psychiatric illnesses. Psychedelic therapy was first studied in the mid-twentieth century before the government criminalized psychedelics and placed stringent restrictions on their use in a research capacity. Now that attitudes toward psychedelics and the necessity of drug criminalization have brought on new reforms, researchers have begun testing again if psilocybin has therapeutic potential. In 2015, astudycategorized alcohol use disorder (AUD) as the most prevalent substance use disorder in the United States though treatment options for patients are still very limited. Despite its ubiquity, Alcoholics Anonymous has a hypothesized success rate of between 3% and 8%. While these statistics have been heavily contested and the premise of Alcoholics Anonymous makes it impossible to track participants’ sobriety, it nonetheless remains that many people are still without effective treatment. This is where psilocybin comes in. Pilot studies testing psilocybin therapy for AUD have demonstrated positive results. During one such study, ten participants with AUD each underwent twelve therapy sessions in a living room-like environment and received psilocybin after the fourth and eighth sessions. After ingesting the psilocybin in capsule form, participants were instructed to lie on a couch wearing eye shades and headphones. They listened to music and were instructed to concentrate on their thoughts and feelings while under the influence of psilocybin. Interestingly, the study demonstrated that both the number of drinking days and heavy drinking days for all the participants decreased throughout the experiment. While this study had a limited sample size, other similar studies have found corroborating results apropos the reduction of substance use and cravings in patients with substance use disorders after treatment with psilocybin. Psychedelic therapy is a promising method of treatment for substance use disorders as well as other psychiatric illnesses. Despite what the government’s archaic and flawed drug classification system says, psilocybin has been shown to be non-habit forming, non-addictive, and quite safe to use for people who desperately need novel treatment approaches. It’s possible that it could be used in the treatment of other substance use disorders with fewer side effects than current treatments. Psilocybin-assisted treatment for AUD holds significant potential and should be tested more thoroughly to determine effective guidelines for its administration.
4 Comments
By Anna Christou
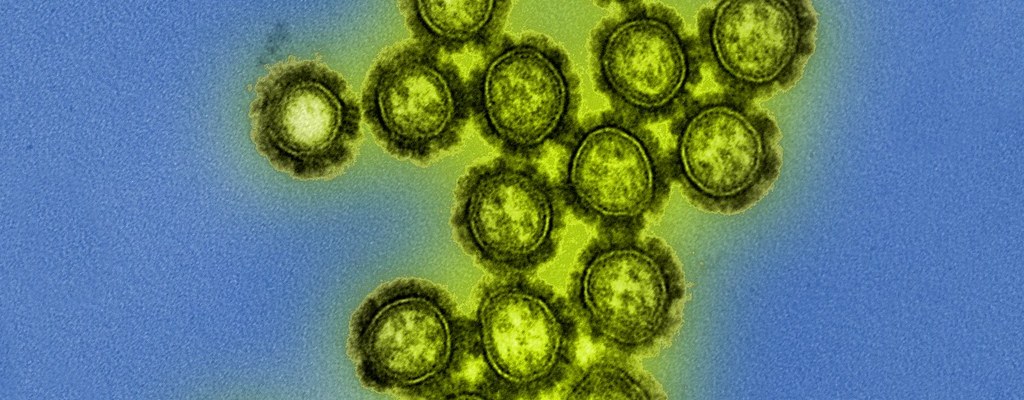
Influenza, commonly known as the flu, is a virus that infects the nose and throat and can lead to sore throat, fever, fatigue, and coughs. The flu is highly contagious and can be spread through the air from sneezing or coughing, or from touching infected surfaces. Each year, 5-20%of Americans contract the flu, leading to 31.4 million outpatient visits and 200,000 hospitalizations annually. Although the flu resolves on its own for most, high-risk patients, such as young children, old adults, or people with chronic illnesses and weakened immune systems, can develop potentially fatal complications, such as pneumonia, bronchitis, or heart problems. The annual flu vaccine is 40-60% effective because it only protects against some strains of the virus, while antiviral medications that reduce the harmful effects of the flu can only treat the illness—not prevent its onset. Therefore, researchers have begun to investigate broadly-neutralizing antibodies as a way to target a wide variety of flu strains at once. Notably, a group of researchers published astudy in Science this past March, outlining their discovery of a pill that can prevent multiple strains of the flu in mice. The Centers for Disease Control and Prevention recommendsthe flu vaccine as a way to protect against the harmful effects of influenza: it can prevent contraction of the virus and, if individuals do become sick, vaccination reduces the severity of their illness. However, the flu vaccine only targets a few specific strains, while new strains continue to emerge. In addition to the vaccine, antiviral drugs, such as Relenza and Tamiflu, can be used to fight the infection and reduce symptoms. One way that antiviral drugs work is by preventing the virus-infected cell from releasing its viral progeny, which could go on to infect other healthy cells. However, these treatments are still not preventive, and reliable prevention techniques still need to be developed. In addition, viruses can develop resistance to antiviral drugs, thus, it becomes even more imperative to develop new methods of combating the flu. Neutralizing antibodies, naturally present in the body, are now being used to prevent the flu. Neutralizing antibodies are carried by immune cells and block the proteins viruses use to invade target cells. Specifically, the antibodies bind to antigens, which are markers of the virus. This renders the virus inactive, since it is now unable to attack and infect host cells. Not all viruses can be inactivated through this approach, since a neutralizing antibody can only bind to specific antigens; however, there are broadly-neutralizing antibodies, which can simultaneously impede a wide variety of virus strains and are, thus, more effective. The fact that influenza-specific, broadly-neutralizing antibodies can be used as a preventive drug is already known. Accordingly, broadly-neutralizing antibodies target the hemagglutinin (HA) stem of the influenza virus, the part of the virus that allows it to enter a host. Since antibodies are large proteins and are difficult to deliver orally, it is necessary to develop smaller molecules in order for this technique to have realistic, practical applications. The researchers who published the aforementioned Science study screened a chemical library to find a small compound that would mimic broadly-neutralizing antibodies and also target the HA stem of the virus. Through in vitro studies, they found that a chemical compound called JNJ7918 could bind effectively to the HA stem and neutralize the influenza virus. The HA stem normally undergoes a conformational change that then triggers the virus to release its genome into the host cell, allowing the virus to reproduce and take over the host. However, JNJ7918 blocks HA and consequently prevents the virus from injecting its genome into the host. The researchers further modified this compound to allow it to bind and neutralize the flu virus more specifically and efficiently. The remodeled compound, named JNJ4796, is more soluble in water and has a lower intrinsic clearance. Intrinsic clearance measures how quickly the liver can metabolize a drug, so a drug with a lower clearance stays active in the body longer. The authors of the paper indicated that increased solubility and lower intrinsic clearance makes this compound more suitable as a drug than JNJ7918. JNJ4796 was also found to bind to and neutralize influenza in vitro, and could protect mice from influenza if administered orally. Since influenza primarily affects the respiratory system, the researchers investigated whether the drug could prevent the flu specifically within the lungs: they found that JNJ4796 could indeed neutralize the influenza infection in bronchial cell cultures. This finding presents a promising method of preventing the flu that can target and attack a broader range of influenza strains. In addition, the development of a small orally-active molecule that mimics a naturally-occurring antibody opens up the possibility of using antibodies as therapies for other diseases, including various types of cancer, rheumatoid arthritis, and multiple sclerosis. Despite this impressive discovery, numerous challenges still exist. Although employing broadly-neutralizing antibodies to fight the flu would allow for more strains of the virus to be targeted, resistance could still emerge. Over time, viruses can develop mutations that confer resistance against these antibodies. Resistant mutants, can then use their selective advantage to infect a larger portion of the population. Nevertheless, the advent of broadly-neutralizing antibodies allows for numerous promising possibilities in flu therapy. By Hannah Prensky, Illustration by Audrey Oh
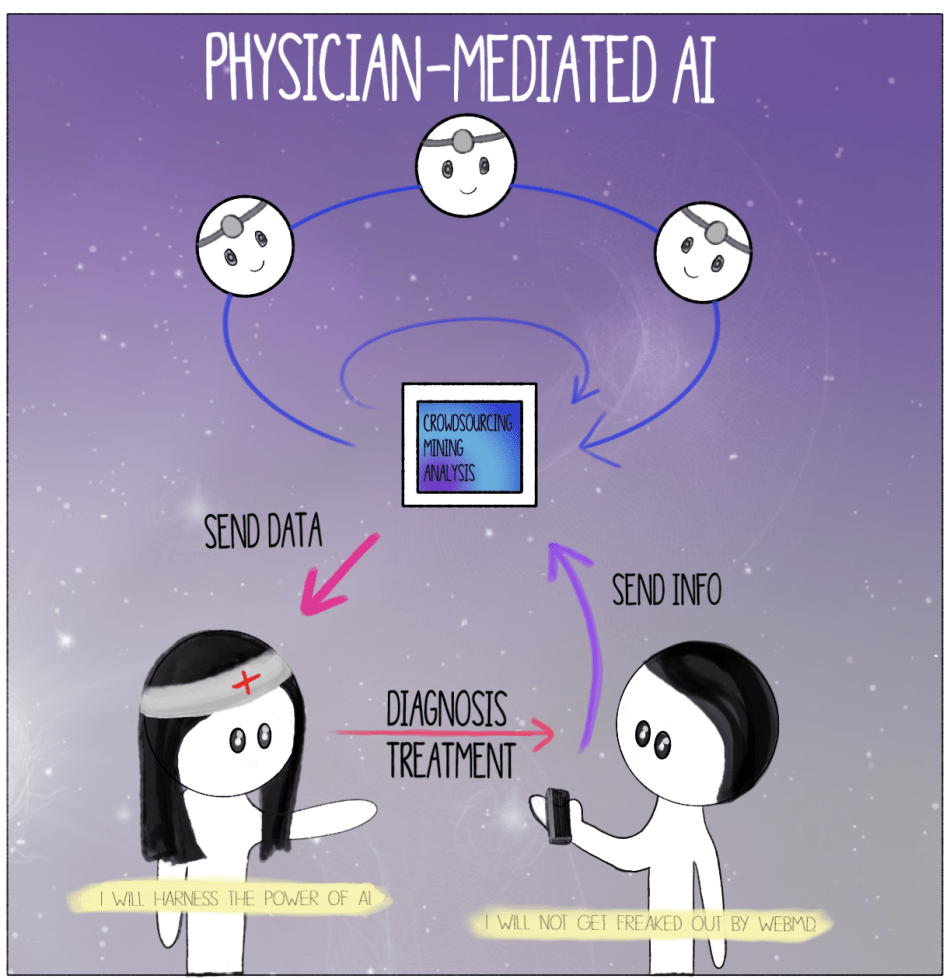
The launching of the Sputnik satellite. The race for space. Laika, the first traveler into the Cosmos. Shepard bringing the American flag into orbit. Since the 1950s, the Cold War propelled generations of astronauts and astronomers to delve deeper into the dark unknown, using rockets fueled by the desire to go further. In the years following Sputnik, the American space agency, NASA, aligned a series of missions like a syzygy of planets in space. During the sixty years since the first venture into the final frontier, human knowledge of space has expanded like the universe during the Big Bang. Now, not only are we sending satellites to look deeper into space; we are sending robots to physically explore other planets. When the Opportunityrover took off for Mars in 2003, the Mars Science Laboratory at NASA aimed to answer some of mankind’s most profound questions. It touched down on the Martian surface with the primary mission of determining whether Mars is, was, or ever will be suitable for life. Opportunity was primarily searching for recoverable water, which is the main indicator of a planet’s potential to sustain life. Water manifests in geological samples that could have been formed from minerals deposited in water-related events, including precipitation, erosion, and sedimentary cementation. Life, as we know it, depends on liquid water for survival; thus, finding water on Mars would be a vital step toward the groundbreaking discovery of life on the Red Planet. Opportunity explored craters, hills, and valleys for an astounding fourteen years. The rover unearthed indications of water through environmental, chemical, and mineralogical analyses of the Red Planet. One piece of evidence supporting the hypothesis that water once saturated Mars arose in the form of small, evenly distributed spherules of the mineral, hematite, on a Martian plain. On Earth, hematite is often formed in areas where hot springs or pools of water flow, which lead scientists to believe the hematite spherules on Mars remained from ancient sources of water. Data and images from Opportunity confirmed that a large body of water once covered the plain. Scientists at NASA are now using clues like these to search for ancient life. On February 13, 2019, NASA declared the Opportunity Mars rover obsolete after almost eight months of silence following a raging sand storm on the surface of the Red Planet. The Martian sand blocked Opportunity’s solar panels, hindering its ability to generate power. NASA lost communications with Opportunity on June 10th, 2018, but scientists remained hopeful that they would regain a signal after the storm subsided in the autumn. Unfortunately, after sending thousands of recovery commands with no response from the record-breaking rover, NASA officially declared the completion of the Opportunity mission in February. The final transmission sent to Opportunity before the mission ended was the song, “I’ll be Seeing You,” by Billie Holiday, delivered to Mars’s Perseverance Valley. Although Opportunity was initially launched from Earth for a planned 90-day mission, it defied all odds and continued to explore for a decade and a half. Since the advent of galactic expeditions in the Cold War era, discoveries and breakthroughs have occurred at a rate few in the 1950s would have thought possible. Despite having sent satellites, animals, humans, and rovers into space, our space achievements are far from over. The hope and progress Opportunity provided to space exploration expanded our curiosity, and offered a unique perspective on humanity’s place in the universe. But more importantly, Opportunity gave us further insight into some of mankind’s most profound questions: What is the nature of life in the universe and does it exist elsewhere? Are we and our planet unique? Humankind has never been satisfied with what we already know. The need to discover more is ever-present. Over time, civilizations have traveled to different colonies, countries, and now, planets. While helping to revive our curiosity for celestial enterprises, projects like the Opportunity rover demonstrate the elegance and elusiveness of the evolving universe. We have no final answers to our age-old questions; the search continues. By Ashley Sun and Sirena Khanna It’s time for your annual check-up. As you enter the doctor’s office you are greeted by the receptionist at the door. Just like last year, you begin your visit with a health questionnaire. You’re happy to discover that this time the survey is given to you on a tablet with a Google Form—no more painful scribbling against a crusty clipboard. You start scrolling through the questions. In the last year, were you or anyone in your family admitted for an overnight stay in a hospital? “No.” Have you ever been diagnosed, treated, medicated, and/or monitored for X, Y, and Z diseases? “No, no, and I have no clue what that is.” You mindlessly tap away at the endless survey, which is still as much a bore as the paper version. At the end, you notice an odd question: do you consent to letting artificial intelligence (AI) use information contained in this survey to better assess patient healthcare? You aren’t quite sure what this means, so you walk up to the receptionist whose bright blue eyes flicker on as you approach. “How may I help you?” it automatically asks. You glance at the name tag. “Hey, NurseBot Janet, can you explain this last question to me?” The robot promptly explains that data from these surveys will be privately stored in your Electronic Health Record and will allow AI to help your physician make a personalized plan for your health. Considering that you have nothing to hide about your health, you consent and press “Submit.” Thank you for your response! NurseBot Janet is not far from the future. In fact, engineers in Japan have alreadydesigned robots like nurse bear and Paroto care for elderly patients by conducting a range of activities, from lifting them off beds to engaging in simple conversation. The potential for artificial intelligence (AI) in the healthcare industry is as vast as your imagination. Dozens of start-ups around the world have created a buzzing field of medical AI. As of now, AI companies have focused on data storage (Google Deepmind Health), crowdsourcing data for research (Atomwise, IBM WatsonPaths), predictive analytics (CloudMedX Health), hospital management (Olive), medical imaging (Arterys, VoxelCloud, Infervision), and personalized care (Bio Beats, CareSkore, Freenome, Zephyr Health). AI has proven to be much better than humans at mining medical records, assessing the success of different treatment options, and analyzing medical scans. With the future of medical AI like Nursebot Janet on the rise, is the healthcare industry going to experience an AI apocalypse,as foretold by Elon Musk? The AI apocalypse may have already begun in your own smartphone. The current market for health-related applications consists of around a quarter million health apps, each of which are relatively sophisticated. These apps often extend far beyond basic diagnostic searches, and include the use of personalized information such as photographs of skin lesions for the detection of melanoma. The sheer detail and convenience that these apps provide have driven consumer demand to new levels. According to a report by Accenture, health app downloads and wearable technology usage have tripled and quadrupled, respectively, in the past four years. The expectations for these tools to deliver high-quality information and care has increased accordingly, as user experience has become a major priority in such apps. With these developments, new issues are emerging concerning the information provided through AI. Studies have been conducted regarding the diagnostic accuracy of apps that focus on melanomas, in particular, and have raised serious questions about the quality of medical information for cancer risks. There are tangible legal and ethical consequencesregarding life-threatening mistakes and how responsibility should be assigned with AI-generated diagnoses. Questions of trust are also being considered, specifically concerning the privacy and security of personal, medical informationbeing stored by private companies. In dealing with these issues, the FDAhas, nevertheless, determined that apps used for diagnosis, treatment, or prevention of disease pose a low risk to the public; as a result, there is minimal regulation at odds with the obvious need for management on health advice that may not always be evidence-based. Ultimately, the main bioethical issues of individualized care, provided through AI-based health apps, are those of accountability, confidentiality, trust, accuracy, and comprehensiveness. Who is accountable for the information provided to the patient? Can you trust an AI company to give you the best health advice? In order to avoid these particular bioethical issues, it may be best for AI health apps to be made specifically for physician use rather than widespread commercial use. Say goodbye to NurseBot Janet. Welcome your living, breathing, human physician. Although smartphone apps may be a great way to empower the patient and give them autonomy over their health, physician-mediated AI use would avoid a multitude of legal and bioethical issues associated with health apps, such as those of regulation and accuracy. How should AI be used as a tool by physicians to personalize patient healthcare? When patients interact with AI apps that are also connected to healthcare providers, their data and a machine-generated diagnosis can be sent to a responsible physician, who would then make the final decisions regarding actual medical care. When many of these patient-AI-physician relationships occur at the same time, the machine learning aspects of AI in apps would augment their decision-making accuracy, which would be repeatedly confirmed by medical professionals, as well. This system would mimic organizations like Human Dxand Figure 1, which are crowdsourcing platforms that rely on solutions proposed by a range of healthcare professionals to solve ambiguous cases. A greater reliance on the opinions of multiple physicians would mitigate inaccurate or overly cautious AI-based recommendations and would aggregate symptoms to create reliable banks of data for future diagnoses. The combined knowledge of physicians and AI will curate more healthcare optionsthat are personalized for the patient. It will also maintain the emotional and humanizing aspect of care in the direct physician-patient relationship. With this paradigm, the physician can ensure personalized healthcare while avoiding the slippery slope of patients self-diagnosing with misinformation. The physician’s involvement also guarantees a level of confidentiality and legal responsibility that currently unregulated health apps do not afford. For example, technologies like Apple’s single-lead ECG featureon their Apple Watch allows the user to print PDFs of their results to share with their physician. AI companies should model their product development under this physician-mediated model, like ADA does, to ensure the most bioethical product. For those skeptical of AI healthcare, rest assured that human doctors will not be replaced by robot clinicians anytime soon. Instead of NurseBot Janet, it’s more probable that you encounter NurseApp Janet, an online smartphone app that stores biometric information and surveys your health for your real-life physician to check each year. Luckily, you agreed to Janet collecting your health information, so the next time you come for your check-up, you won’t need to answer the boring and generic patient questionnaire. Through the app, AI has gathered the answers to these questions, while your healthcare provider has consulted with a crowd-sourced sharing platform to come up with accurate and comprehensive healthcare advice for your mysterious disease. On your next visit to the doctor’s office, you’re glad to see that NurseBot Janet has been replaced by—you take a closer look at the nametag—Janet, a human this time. For now, the AI apocalypse can be averted by keeping humans in charge of your healthcare.
|
Categories
All
Archives
April 2024
|