|
By Tiago Palmisano
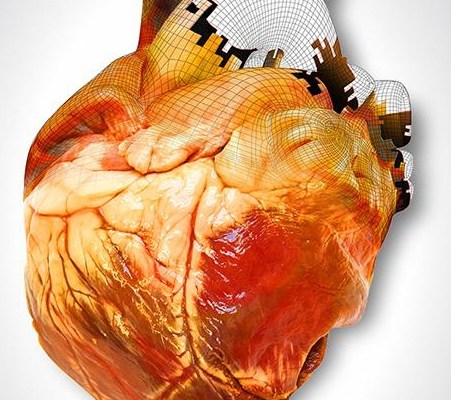
Integration of biological material with the technology of 3-D printing is beginning to redefine the limits of medical treatments and patient care, and will eventually change the ways that doctors treat patients. The last two decades have seen an explosive rise in the applications of 3-D printing–the process of making a three-dimensional object using a virtual design. 3-D printers use CAD (Computer Aided Design) files to deconstruct a product into thousands of successive 2-D layers, fabricating an object one layer at a time. Although the technology originated as a small manufacturing niche in 1986, it has grown substantially and is now commonly used to produce low-volume objects such as toys, wristwatches, and airplane parts. The majority of 3-D printers use some type of metal alloy, plastic, or powder to form each 2-D layer. Typically, a laser or heated nozzle is programmed to selectively harden the liquid or powder material into the desired shape out of the initially homogeneous substance. Recently however, more sophisticated printers and software have facilitated the use of increasingly complex materials such as biological cells. These advancements have ushered in a new age of “bioprinting” which is already transforming traditional medical care. Tissues fabricated with 3-D bioprinters, such as heart, skin and cartilage structures, are currently used as transplant components. In the past, fractured jaw and hip bones have been reconstructed using traditional material, such as titanium, but bioprinting is different. A biological 3-D printer generates actual tissue; the printed materials don’t mimic body parts, like metal, but rather are realcells, identical to the ones found in a human body. Scientists at Princeton University 3-D printed a functioning human ear using skeletal and cartilage cells.The first step to 3-D printing tissues is obtaining the digital file needed for the printing software. This is achieved with techniques such as computed tomography (CT) and magnetic resonance imaging (MRI) that gather extensive information of the tissue’s complex three-dimensional biological framework. Next, the 3-D printing software uses this data to carefully arrange living cells into the 2-D layers that form the intended shape, resulting in biologically compatible living tissue. In this case, “biologically compatible” means that the tissue does not induce a negative, inflammatory response in the body, making it ideal transplant material. A crucial part of the process is the selection of cells. Usually, bioprinters are loaded with stem cells–undifferentiated cells that have not yet been become specialized (an example of a specialized cell would be a muscle or blood cell). Because of this, stem cells can develop into the specific role required for the desired tissue. The chosen cells are also normally paired with a biologically compatible polymer for structural support. Although 3-D printing has successfully produced certain tissues, the ability to fabricate entire organs is still a vision of the future. Organs are extremely sophisticated structures with dozens of distinct cell types and functions, and just putting the right cells in the right shape usually isn’t enough to make a working organ. An organ must be able to deal with the intricate signals of the body and the intense stresses of the environment, such as heat or pressure. Despite this, the leap to full-fledged body parts such as organs may not be too far off. The amount of scientific literature referencing bioprinting has tripled in recent years, and research spending has increased significantly. Even if 3-D printed organs aren’t used in human transplants for many decades, other invaluable applications exist. Testing new drugs on fabricated organs could reduce the need for animal testing, and allowing medical students to train for surgeries using printed body parts would provide better preparation and lower patient risk. Additionally, the technology being developed for 3-D bioprinting may lead to other medical innovations. For example, labs at the University of Wollongong in Australia have created a handheld “bio pen”—a surgical tool that can deposit stem cells directly to damaged cartilage and bone. This provides doctors with a precise, efficient way to reconstruct certain tissues without the need to use cellular materials from other parts of the patient’s body. Indeed, the possible applications of 3-D bioprinting seem almost limitless. Quickly made and specific transplant material will vastly change how doctors heal and save lives. Though 3-D printed organs are not yet a reality, we may see them in the not-so-distant future. The need certainly exists, as over 500 people die waiting for transplants every month. Additional funding and research have facilitated great strides in the field of bioprinting. Such advancements intimate that a revolution in medicine is imminent, and given the improvements it may provide in patient care, it can’t come soon enough.
0 Comments
Leave a Reply. |
Categories
All
Archives
April 2024
|