The Concourse of Traditional Chinese Medicine and Western MedicineBy Sirena Khanna Traditional Chinese Medicine (TCM) is an ancient method of healing founded upon the idea of Qi. Qi, written as 气 and pronounced like the “chi” in “chia seeds,” means energy in Chinese. In English, the word “energy” derives from words associated with force and vigor, but anyone who has taken general chemistry or physics knows that the concept of energy has much deeper underpinnings in nature itself. Energy simultaneously builds and destroys the universe; from the microscopic interactions between atoms in a water molecule, to the giant nuclear explosions that rocked the end of World War II, energy determines the order of life— for good or bad. In Chinese, the word for energy captures its fundamental role in everyday life. The character Qi (气) appears in the words for “gas” (气体), “air” (空气), “odor” (气味), and “weather” (天气), among many others. The character 气 is written using the “air/gas” radical, so the idea of a disseminating energy is embedded in the way it is written, too. The deeply-rooted and rich connotations of Qi elevate the idea of energy in the Chinese language to something more accurately translated as vital energy or life energy. Similarly to the matter-energy construct in physics, Qi in Chinese medicine explains what binds the universe together. Qi connects every dimension of life: physical, mental, and spiritual; as such, TCM practices focus on promoting and maintaining the flow of Qi in a person’s body, mind, and spirit. Being able to practice TCM relies on an understanding of Qi, and since there are many ways to qualify this energy, TCM practitioners need to be well-versed in recognizing its different aspects. The overarching classification system is known as yin and yang (阴阳); yin is associated with being cold, feminine, and light, while yang is associated with being hot, masculine, and heavy. Good health, according to yin and yang, is a balance between these complementary forces. 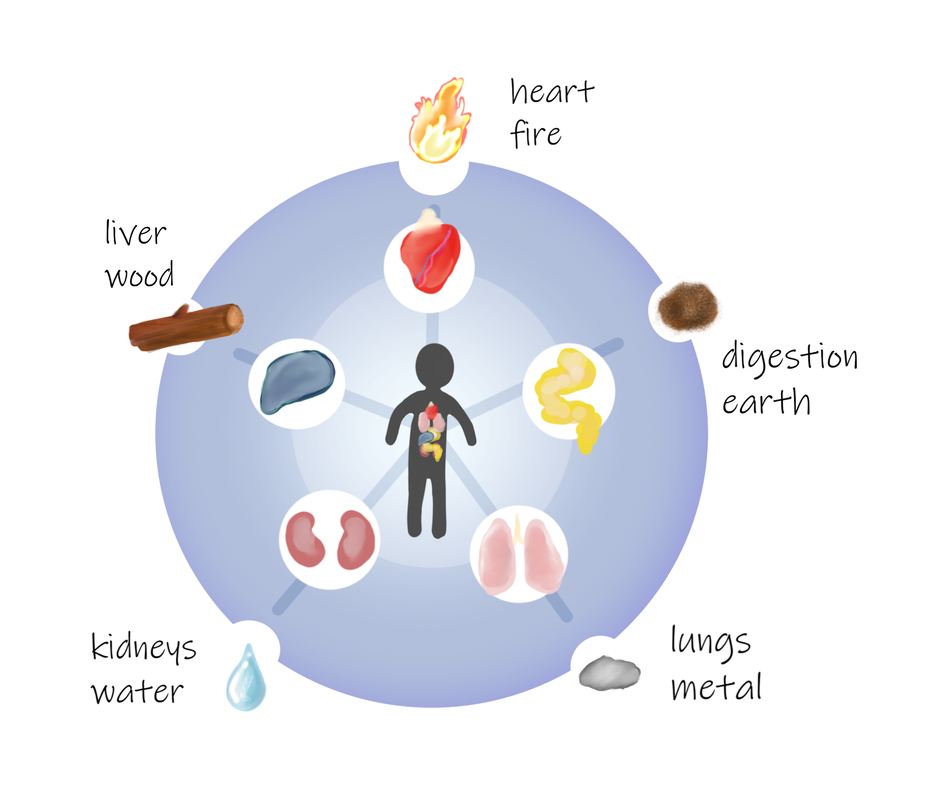 While yin and yang forms the basis of TCM and Chinese philosophy, this overarching dynamic can be further broken down into the Theory of Five Elements, in which certain elements represent yin and others embody yang. This theory also attributes a Qi to each of the five vital organs; for example, there are a Liver-Qi, a Kidney-Qi, and a Heart-Qi. Each organ-Qi is associated with one of the five elements: wood, fire, earth, metal, and water. According to yin-yang and the Theory of Five Elements, illnesses are a direct result of an imbalance in or excess of Qi. For example, depression is most commonly associated with an imbalance in Liver-Qi. When a patient seems depressed, a TCM practitioner might address their Liver-Qi stagnation through acupuncture and/or a prescription of herbal remedies. TCM texts, like Western Medicine textbooks, house a vast amount of information that help the practitioner devise a proper treatment. Some of these texts are thousands of years old, such as the 2,200 year old Huang Di Nei Jing. Modern TCM texts compile empirical evidence not only from ancient TCM texts like Huang Di Nei Jing but also from modern TCM practices. The Five Flavors Theory summarizes centuries of empirically determined herbal remedies. The theory classifies each herb under five different flavors and a temperature, either cold or hot. There are five tastes— sweet, salty, sour, bitter, and acrid (spicy)—each of which corresponds to an element in the Theory of Five Elements. Imbalances in Liver-Qi, for example, are treated with sour-tasting and cooling herbs because these herbs have relaxing and fluid-retaining properties. TCM posits that plants such as Aconitum (commonly known as aconite or monkshood) fall under this criteria, so Aconitum allegedly nourishes the liver and helps blood circulation. Altogether, yin and yang and the Theory of Five Elements are used to classify the different qualities of Qi, and in doing so, these systems form the cornerstones of diagnosing and treating illnesses within TCM. To those brought up with Western Medicine (WM), the TCM system of diagnosis and treatment seems radically different. Is taste really a good indicator of medicinal effect? Does the TCM approach to Qi miss the mark completely? The relatively recent emphasis on evidence-based research has spurred studies into the efficacy of TCM. Although much of this research is in its infancy, the preliminary results show why the thousands years-old system of TCM works on a physiological to molecular level. In order to address Liver-Qi stagnation, researchers at the Beijing University of Chinese Medicine created a rat model of depression to study the biological basis of Liver-Qi dysfunction. In the study, the researchers identified three genes in the liver associated with depression; they also proved that treatment with the Chinese herb Si Ni Tang (scientifically known as Aconitum) helped improve depression-related behaviors in the rats. The specific mechanisms that alter the expression of these depression genes in the liver were not revealed, but, at the very least, this study confirms the relationship between liver dysfunction and depression. Another common area of interest is the role of Chinese herbs in treating diseases like diabetes and diseases of the nervous system, such as neuropathy. Neuropathy is a broad category of disorders caused by the degeneration of the nervous system. Peripheral neuropathy (PN), in particular, is a condition that results from damage to the peripheral nervous system. PN is a common complication of diabetes mellitus (DM). 60 to 70 percent of patients with diabetes also have neuropathy, a condition specifically referred to as diabetic peripheral neuropathy (DPN). In America, around 20 million people have DPN, and although the prevalence of DPN has not been measured in China, around 114 million people there have DM.  Traditional Chinese Medicine (TCM) uses both acupuncture and herbal remedies to treat PN disorders such as DPN. In 2012, researchers at the Peking Union Medical College Hospital verified the use of Astragalus, Salvia, and yam in such treatment. In their study, they studied the effects of these herbs on Schwann cell myelination and neurotrophic factors, which are important players in maintaining and regenerating neurons. Although the exact mechanisms of Astragalus, Salvia, and yam on the nervous system are unknown, the study nonetheless demonstrated that these Chinese medicines promote nerve repair and regeneration. Slowly but surely, evidence-based research is shedding light on the scientific basis of what has been known through trial and error in TCM for thousands of years. A promising example of the concourse of TCM and WM appeared in a 2017 study on the use of acupuncture in hospital emergency rooms. The study, published in the Medical Journal of Australia, showed that acupuncture is an effective medication in treating acute pain for ankle sprains and lower back pain but that its analgesic effects take around an hour to manifest; however, once its full effects set in, the pain relief was comparable with that of pharmacotherapy. Although research into TCM is just beginning, the modernization of TCM is well underway. In the US, the National Center for Complementary and Alternative Medicine (also known as the National Center for Complementary and Integrative Health, or NCCIH) was established in 1998 “to define, through rigorous scientific investigation, the usefulness and safety of complementary and alternative medicine interventions and their roles in improving health and health care.” The center has a budget around $120 million US dollars, an investment that speaks to the United States’ interest in pursuing integrative medicine. On the international stage, in 2008, the World Health Organization (WHO) supported an international agreement called the Beijing Declaration that promotes the preservation of traditional medicine in national healthcare systems across the world. This declaration is representative of the global impetus towards integrative medicine. In 2016, China further propelled the shift toward evidence-based research into TCM by passing new legislation that expanded its funding. As Article 8 of the Law of the People's Republic of China on Traditional Chinese Medicine upholds, “The state supports TCM scientific research and technical development, encourages innovation in TCM science and technologies, shall popularize and apply TCM scientific and technological achievements, protect TCM intellectual property rights, and enhance TCM scientific and technical level.” Overall, the legislative push towards researching TCM in a scientific setting bodes well for its integration into WM. In a yin and yang fashion, TCM and WM balance each other’s extremes. The use of randomized clinical trials and biomedical research can bring TCM up to speed with WM modern standards, while TCM can teach WM the overarching, holistic approach of traditional medicine. An important application of this mutualistic relationship between TCM and WM is in pharmaceuticals. Pharmaceutical research often focuses on a reductionist method by singling out compounds from herbs to sell as drugs. However, the one-drug-one-disease philosophy is questionable. Current research suggests that herbal medicine, including those from TCM, has synergistic effects, so individual active ingredients work together to create a greater effect and should not be isolated and prescribed on their own. TCM can complement the rigid, sometimes narrow-minded views in WM with a fluid, personalized treatment. For example, a Western doctor might prescribe vitamin supplements to someone with neuropathy if the doctor thinks the disease is caused by a vitamin deficiency. In comparison, TCM practitioners treat the entire body with multiple herbal remedies in order to balance the flow of Qi. TCM’s holistic approach to disease explains why acupuncture is also a big part of treatment. Disease is a complex interaction of many biological systems, so the entire person— not just one type of molecule— should be treated.
The best of both worlds would be a combination of WM and TCM. Integrative medicine could yield the best diagnoses since it combines TCM pattern classifications alongside biomedical diagnoses. Many patients turn to TCM clinics for this reason: when WM had no cure, TCM was the next best option. Treating TCM as a last resort reveals the myopic attitude many people in the United States have toward alternative medicine. Yet, TCM might be able to treat certain diseases better than WM, and unfortunately patients only discover its virtue after going through everything WM has to offer. Moreover, TCM is rooted in preventative, non-invasive medicine, so the goal is to maintain balance in Qi before major diseases ensue. In this regard, TCM is not only more cost effective but also better for the patient’s health because it potentially prevents disease altogether. The main deterrent to TCM integration in WM is the lack of awareness and the stigma against Chinese medicine. Most insurance companies do not offer coverage for TCM acupuncture and herbal remedies due to safety and liability concerns; these concerns are mostly unfounded because licensed TCM practitioners must undergo rigorous training and obtain a formal license to practice medicine, just as WM doctors do, too. But, as research continues to support TCM practices and as patients turn to alternative medicine, demand could carve out a new space for TCM in the Western healthcare market. As it turns out, through alternative medicine, WM and TCM have the potential to complement each other and strike balance within the healthcare system, which at the moment could use a bit more yin and less yang.
1 Comment
Thanks for helping me understand that an integrative medicine center would be able to diagnose certain patterns and their classifications better. I can imagine how helpful it would be for my sister to go to a center like that here in Schaumburg, Illinois this weekend to get herself checked. She has been talking about the pain in her nails which seems not related to ingrown nails at all.
Reply
Leave a Reply. |
Categories
All
Archives
April 2024
|


