|
By Kendra Zhong
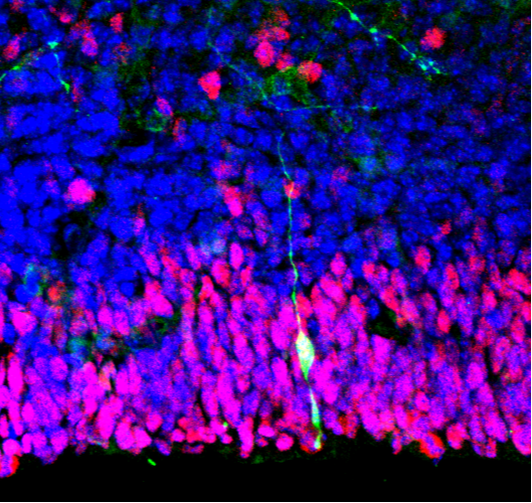
After suffering a stroke in 2009, Jim Gass was confronted with a flaccid left arm and weak left leg. He then decided to take what many would consider a dream vacation: traveling to various countries in North America, South America, and Asia. However, Gass wasn’t chasing tourist traps—he was chasing promises of recovery from his stroke. The apparent successes of several specialized medical clinics in Mexico, Argentina, and China gave Gass hope that treatment via stem cell implantation therapy would cure him. Unfortunately for Gass, he became further paralyzed from the neck down. Despite continuous efforts by the Food and Drug Administration to shut down facilities administering scientifically unverified and potentially dangerous treatments leading to more cases like Jim’s, hundreds of stem cell clinics still exist in the United States [2]. At the same time, research on stem cell transplantation has come to the forefront of science for its promising therapeutic potential. Today, Columbia University is exploring the vast possibilities of stem cells. It has recently established the Jerry and Emily Spiegel Laboratory for research on brain stem cell replacement therapy in addition to ongoing stem cell transplant treatments at the medical center. The Herbert Irving Comprehensive Cancer Center (HICCC) at CUMC currently conducts autologous and allogeneic stem cell transplants, the former referring to the process of collecting stem cells from the patient’s blood and the latter relying on a donor’s stem cells, both of which can be used to grow new bone marrow tissue in the patient. HICCC has also shown dedication to improving the safety of such procedures. Its research focuses particularly on therapeutic combatants against graft-versus-host disease, a prevalent and life-threatening complication following allogeneic transplantation, in which the patient’s immune system rejects the “foreign” bone marrow and effectively works to destroy it. Other institutions are also recognizing the promising results of stem cell treatment, but only if safe implementation is realized. In a recent clinical trial conducted by researchers at Stanford University’s School of Medicine, eighteen participants who had suffered a stroke six months to three years prior received injections of adult human stem cells into the brain. While more than thirteen patients developed short-term headaches after the procedure, no long-term side effects were observed. The researchers also found a significant overall improvement on the motor-function component of the Fugl-Meyer Assessment, the standardized index used to assess recovery of stroke victims, at six and twelve months after injection. The stem cells had apparently increased patient mobility. These results important due to their consistency amongst all the trial participants, regardless of the severity of stroke, and equal application to an older demographic (the average age of the patients was 61). These encouraging results have inspired the organization to devise a subsequent trial with a greater number of participants. Their research also aims to find new and improved methods for bone marrow transplantation. Patients’ blood stem cells must be killed before transplantation of new stem cells, but current treatments using chemotherapy or radiation therapy to kill existing stem cells are toxic to the liver, reproductive tissues, and brain, making stem cell transplants extremely dangerous. Yet, researchers at Stanford University’s School of Medicine recently found that attaching antibodies to c-kit and CD47—two marker proteins of blood stem cells—allowed macrophages to target and destroy the blood stem cells in mice. This technique makes blood stem cell implants both safer and easier to execute. However, as research progresses towards realizing promising treatments, the cost of current stem cell clinic practices push back—Mr. Gass paid almost $300,000 for his injections just a few years ago. Other transplantation treatments have been estimated to cost upwards of $800,000. Thus, as stem cell transplants become more advanced, safe, and common in the US, the next criteria to consider should be practical applicability and accessibility. Kendra is a Columbia College freshman studying biology and chemistry. She’s a staff writer for the Columbia Science Review.
1 Comment
12/13/2023 04:37:24 am
This Blog Is Very Helpful And Informative For This Particular Topic. I Appreciate Your Effort That Has Been Taken To Write This Blog For Us.Best hospital for brain stroke treatment in hyderabad, Recovery after brain stroke, Physiotherapy for brain stroke patient, Physiotherapy after brain stroke, Brain stem stroke rehabilitation, Brain stroke center in Hyderabad, Stroke brain damage recovery, Brain stem stroke recovery, Traumatic brain injury stroke recovery, Physiotherapy for brain stroke<a href="https://curerehab.in/Brain-Stroke-Rehabilitation"> physiotherapy in Hyderabad </a>
Reply
Leave a Reply. |
Categories
All
Archives
April 2024
|