|
By Mariel Sander
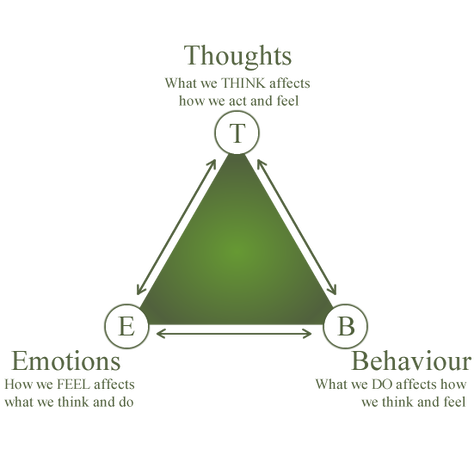
When considering treatments for mood disorders like depression or anxiety, people usually think of medications like Prozac or Zoloft - medications that necessitate a lifelong dependence on fluorescent orange bottles and daily pills. On the other hand, while psychotherapeutic treatments exist, individuals often imagine them as ineffective, unscientific, and outdated. Last fall, my friend made the decision to take a year off from school to focus on improving his mental health. He enrolled in a program focused primarily on teaching participants how to implement a kind of psychotherapy called cognitive-behavioral therapy (CBT). CBT is a relatively new, promising psychotherapy that’s been shown to promote positive neural changes and long-term mood improvements with the same efficacy as pharmacotherapy. As the name suggests, CBT is a combination of cognitive and behavioral therapeutic methods. There is a marked focus in understanding one’s own cognitive processes and how these habits affect behaviors. This approach is often visualized in a triangle schematic in which emotions, thoughts, and behavior are interconnected. What differentiates CBT from other psychotherapies is its emphasis on patient-led, practical problem-solving. A traditional psychotherapeutic approach helps the patient search for underlying causes of their illness by examining possible childhood traumas and influences. However, in CBT, the therapist simply teaches the patient to address their difficulties in an immediate and self-sufficient manner. One common technique taught in CBT involves becoming more aware of negative patterns of thought called “cognitive distortions.” One cognitive distortion would be “mind-reading.” Let’s consider an example of this distortion. Your close friend cancels on your plans to see a movie together. If your most immediate thought is “they must have canceled because they don’t like me and think I’m weird,” you’re falling into the pattern of “mind-reading.” You think you know what someone else is thinking about you, even when in reality there could be many other reasons they chose to cancel. In CBT, a therapist would teach the patient about these cognitive distortions and how to become more aware of them. CBT focuses not on delving into the patient’s past, but on finding future solutions. The patient must be self-motivated and willing to change aspects of their thoughts and behaviors to cultivate a better, healthier mindset. Over the years, CBT has been effective in treating more than just depression. It has also been proven to have the same efficacy as and lower rates of relapse than pharmacotherapy for anxiety, post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), and phobias. A 2005 study found that PTSD patients typically have trouble with social cognition, particularly in the areas of empathy and forgiveness. After CBT, the patients showed increased activation in the left medial temporal gyrus and posterior cingulate gyrus, two parts of the brain linked to empathy and forgiveness, without the use of traditional medications. Additionally, CBT was shown to be effective for treating OCD in a study where a group of afflicted individuals underwent CBT, while another group underwent the traditional pharmaceutical treatment with fluoxetine. Neuroimaging showed that both CBT and pharmaceutical groups displayed a decrease in activity in the right caudate nucleus, which consequently reduced the expression of OCD symptoms. There was, however, a small difference noted: the group treated with fluoxetine demonstrated a decrease in thalamus activation, while the CBT group did not. However, there haven’t been definitive studies linking decreases in thalamic activation to the improvement of symptoms. While CBT does have real, quantifiable benefits, there are some critical faults, as reported by my friend. “It was exhausting and daunting to think that from now on I had to change my thoughts and second guess myself,” he said, after weeks of working with therapists and learning CBT techniques. “It definitely isn’t easy.” As my friend's experience suggests, CBT requires that patients invest an incredible amount of work, persistence, and self-motivation to ameliorate their disorders. Nevertheless, research suggests CBT can be effectively implemented even in cases of severe depression. In these cases, CBT is often also combined with medication to achieve more rapid results. Despite CBT’s proven efficacy, most state mental health systems have neither instituted nor funded it. This could be due to the misconception that medication is the only route to promoting positive neural changes or that merely forming different habits, as in CBT, doesn’t substantially affect the brain. CBT provides a promising route to a more patient-focused form of treatment, providing insight into the patient’s own thought patterns and allowing them to better understand, and thus improve their overall mental health. “With lots of practice, the skills I learned throughout therapy have changed my overall mood in drastic ways,” said my friend, upon completing his combined CBT and pharmacotherapy program. “Surprisingly, CBT has been life-changing for me.”
0 Comments
Leave a Reply. |
Categories
All
Archives
April 2024
|