|
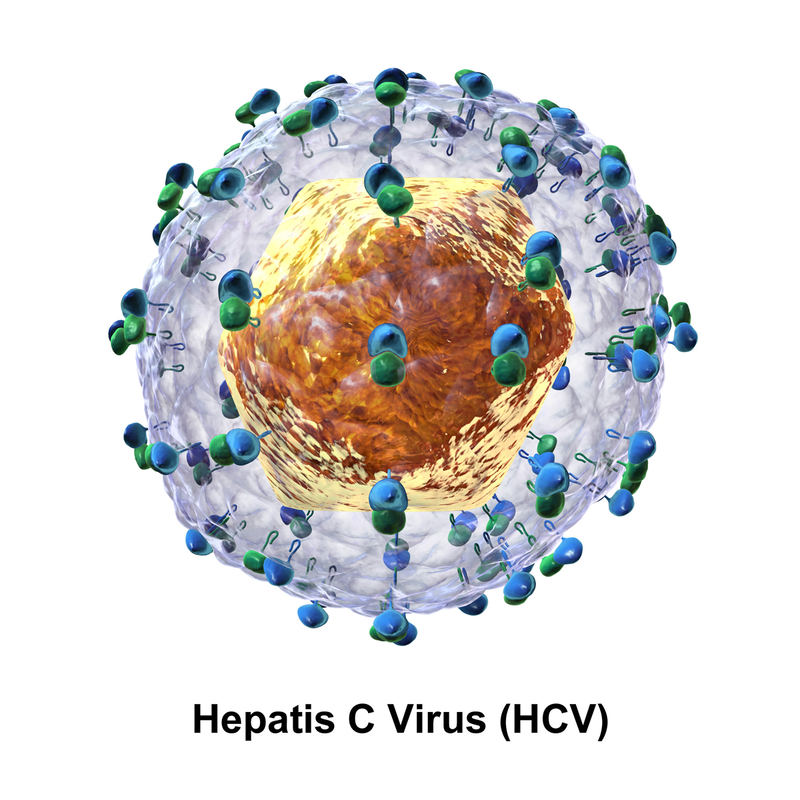
By Eleanor Lin Today, thanks to mandatory screenings, people are able to safely receive life-saving blood transfusions to replenish blood loss from traumatic injuries. That was not the case in 1667: the first documented blood transfusions to humans went horribly wrong, resulting in two deaths. Unbeknownst to physicians at the time, it is extremely dangerous to transfer blood from one person to another without checking to make sure that their blood types match, and that the donor's blood does not carry any pathogens (i.e. harmful particles such as viruses). If the donor's blood type does not match the recipient's, it could trigger a fatal immune response in the recipient; if pathogens are present in the donor's blood, they could create serious disease. It was not until the 1800's that scientists began again to seriously investigate blood and its utility in medical treatments. In the absence of strict regulatory guidelines and full knowledge of the causes of infectious diseases, major health risks persisted for blood transfusion recipients. For instance, "until the 1960s, exposure to blood from infected individuals was a major health hazard, with up to [a] 30% risk of chronic hepatitis following surgery or multiple blood transfusions." That shocking statistic was cited by the Nobel Assembly in its press release announcing that Harvey J. Alter, Michael Houghton, and Charles M. Rice had won the 2020 Nobel Prize in Physiology or Medicine "for the discovery of the Hepatitis C virus." Before diving into Alter, Houghton, and Rice's three-decade search for this viral culprit, it might help to understand the nature of hepatitis itself. "Hepatitis" simply refers to liver inflammation, which can be caused by factors such as alcohol abuse, toxin exposure, autoimmune disease, or, most commonly, viral infection. Hepatitis A virus (HAV) and Hepatitis E virus (HEV) are transmitted through water and food and cause acute (i.e. sudden) disease, which is usually resolved in life-long immunity. HBV, HCV, and HDV, however, are transmitted through bodily fluids (such as blood) and cause chronic (i.e. long-lasting) disease, which may lead to liver failure or liver cancer. In 2016 alone, an estimated 96% of 1.4 million fatal viral hepatitis cases worldwide were caused by the type B and C viruses. Because chronic hepatitis has a long incubation period, during which symptoms are mild and effectively under the radar, an infected person is at high risk of unknowingly transmitting the disease to others. Thus, before the advent of hepatitis screening tests, blood transfusion recipients, health care workers, and people addicted to injected drugs were all at especially high risk of chronic hepatitis infection. Even with screening tests, HCV remains prevalent today: the WHO estimated that in 2015, 71 million people, or 1% of the world population, had a chronic Hepatitis C infection. The discovery of the Hepatitis B virus (for which Baruch Blumberg was awarded the 1976 Physiology or Medicine Nobel) was followed closely by the development of tests for Hepatitis A and B, as well as a Hepatitis B vaccine. But patients continued to develop chronic hepatitis after blood transfusions. What could be the culprit behind these particular cases of "post-transfusion hepatitis"? Here is where our first Nobel laureate, Harvey J. Alter, enters the story. Having worked with Blumberg on identifying HBV, Alter continued researching post-transfusion hepatitis in the 1970’s. He and his colleagues used the newly developed HAV and HBV tests to rule out HAV and HBV as the causes of a significant portion of post-transfusion hepatitis infections. These mystery cases were dubbed with the frustratingly non-descriptive name "non-A, non-B hepatitis," or NANBH for short. NANBH caused chronic infections more frequently than HBV, yet its carriers usually showed no signs of infection: a deadly combination. Alter suspected that a distinct virus was causing the NANBH cases, but how could he prove it experimentally? His breakthrough came from using a "primate model" of hepatitis infection. He demonstrated that blood serum from human NANBH patients was sufficient to cause chronic hepatitis in chimpanzees. (Serum is a product of processing blood plasma, the liquid constituent of blood.) This implied that a yet-to-be-identified, blood-borne virus caused NANBH. Alter also uncovered clues about the virus's structure, such as the fact that it included lipids. Lipids are biological building blocks which help make up the viral envelope, a protective coat found in many viruses—including, as has since been confirmed, Hepatitis C. In order to more precisely identify and classify the NANBH virus, however, scientists still needed to isolate and characterize its genome. Like all viruses, the virus for NANBH had to have a genome, a sequence of nucleotides encoding a unique set of instructions for its own structure and replication. In the 1980's, Michael Houghton successfully isolated this genome from NANBH-infected chimpanzees. He and his colleagues named the virus Hepatitis C and identified the material making up its genome as ribonucleic acid (RNA), allowing them to classify the virus. They used their newfound knowledge of the HCV genome to develop a test for HCV antibodies. Since specific antibodies are proliferated by the immune system to fight specific infections, the presence of antibodies for a pathogen (such as HCV) can serve as evidence of past infection by that pathogen. Houghton's test found HCV antibodies in NANBH patients, strengthening evidence for the association between HCV infection and NANBH. Yet in order to establish a cause-and-effect relationship between HCV infection and NANBH, science still demanded experimental evidence that the virus, by itself, could create the disease's symptoms. To do just that, Charles M. Rice and his colleagues, as Alter had previously done, used a primate model. Rice identified a region of the HCV genome which was crucial to the virus's replication. He demonstrated that infection with engineered genomes that included this key region caused chronic hepatitis and HCV proliferation in chimpanzees. Thus, Rice's work completed the evidentiary chain. There was finally a definitive explanation for those mystery cases of chronic hepatitis that Alter had characterized decades earlier: the Hepatitis C virus. In addition to testing, Alter, Houghton, and Rice's work laid the foundations for the development of antiviral drugs, making HCV-induced chronic hepatitis curable. However, high costs and lack of adequate public health infrastructure for screening remain barriers to testing and treatment in many places, and an HCV vaccine has yet to be developed. Nevertheless, science offers hope in unexpected ways: Remdesivir, now repurposed for COVID-19 treatment, originated as an HCV antiviral. Who can predict where future discoveries may take us?
0 Comments
Leave a Reply. |
Categories
All
Archives
April 2024
|